A stent thrombosis is a blood clot that forms within a coronary stent. It can be a complication of stent placement to open a narrowed artery.
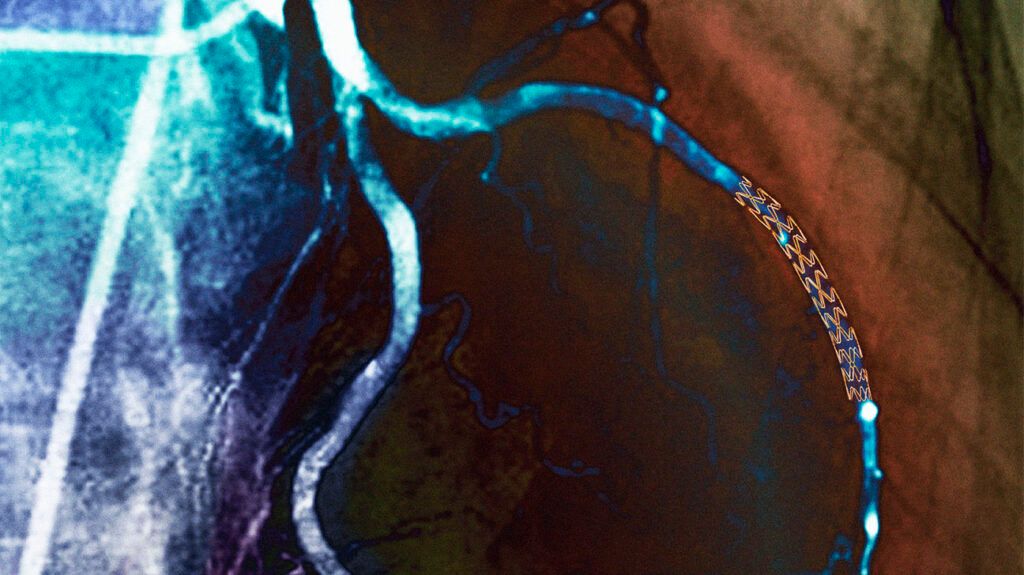
A coronary stent is a mesh tube that opens a narrowed or blocked artery to restore blood flow to the heart.
A stent thrombosis is a severe complication of stent placement that can occur with percutaneous coronary intervention (PCI).
A stent thrombosis
- chest pain or discomfort
- pain or discomfort in the arms, back, stomach, neck, or jaw
- shortness of breath
- feeling lightheaded or dizzy
- nausea
- sweating
If people experience these symptoms, call 911 immediately.
A stent thrombosis may occur
Delayed healing, which may occur with a drug-eluting stent, may also play a role in stent thrombosis. A drug-eluting stent is coated with medication that prevents tissue from growing and continued narrowing of the artery.
There is a
Experts recommend continuing dual antiplatelet therapy (DAPT) for
One of the
Other risk factors for stent thrombosis include:
- diabetes
- kidney impairment
- acute coronary syndrome
- reduced left ventricular ejection fraction, which is a problem with how the heart muscle contracts
- non-ST elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI), which are both types of heart attack
- the extent of coronary artery disease
- the size and positioning of the stent
There is no significant association between the type of stent and the risk of stent thrombosis, though the type of stent may affect the timing of stent thrombosis.
Experts associate an earlier occurrence of stent thrombosis around
To diagnose stent thrombosis, a doctor will take a medical history and conduct a physical examination to assess any symptoms. They may carry out tests to check the heart,
- electrocardiogram (EKG), which measures the electrical impulses of the heart to see how it is beating
- echocardiogram, which is an ultrasound to show how well the heart muscle is working
- cardiac enzymes test to measure the levels of enzymes the heart releases, which can indicate problems with the heart
Doctors may use intravascular ultrasound (IVUS) or optical coherence tomography (OCT) to examine the stent and identify what is causing the stent thrombosis.
IVUS uses a catheter with an ultrasound to create an image within the blood vessels to check for any narrowing or blockages.
OCT also creates images within the blood vessels, but it uses light rather than sound waves to create the images.
Doctors
Aspiration thrombectomy is a surgical procedure that uses a catheter and a device to suction and remove a blood clot from a stent.
In angioplasty, a doctor guides a catheter through the blood vessels to the blockage and inflates a small balloon to open the narrowed passage.
Doctors may place an additional stent to prevent the recurrence of a stent thrombosis.
Doctors
Without treatment, stent thrombosis
Treatments for stent thrombosis also have a risk of complications similar to those with PCI, including:
- bruising
- hematoma, which is the leaking of blood from a blood vessel
- pseudoaneurysm, which is a pooling of blood due to an injured artery
- retroperitoneal hemorrhage, bleeding into the retroperitoneal space, which is behind the lining of the abdomen
- arrhythmia or irregular heartbeat
- impaired kidney function
- recurrence of a blood clot
- infection
- ischemic stroke
- heart attack
Read about PCI for heart disease.
Taking DAPT exactly as a doctor prescribes may help prevent stent thrombosis. According to a
There is a
Close monitoring within
People will need to seek emergency medical attention if they have chest pain, shortness of breath, or any other symptoms of acute coronary syndrome following a stent placement.
Stent thrombosis is a rare but severe complication of coronary stent placement, with a mortality rate of
Stent thrombosis
Cardiovascular health resources
Visit our dedicated hub for more research-backed information and in-depth resources on cardiovascular health.
Stent thrombosis is a blood clot that forms in a coronary stent following percutaneous coronary intervention (PCI). A stent thrombosis can be life threatening without prompt treatment.
Treatment involves removing the blood clot and reopening the stent. Antiplatelet therapy may help reduce the risk of stent thrombosis.
If people experience any chest pain, shortness of breath, or other concerning symptoms following stent placement, they should seek medical help immediately.
