- Multiple factors contribute to someone’s risk of developing cancer.
- Obesity is one risk factor that can increase the risk of some cancer types.
- Researchers are interested in discovering strategies that will best help to decrease someone’s risk for obesity-related cancers.
- A new study found that people with type two diabetes who were treated with glucagon-like peptide receptor agonists were at a reduced risk for 10 different obesity-associated cancers.
Obesity and type 2 diabetes are common conditions that can pose a risk to people’s health. Diabetes treatment approaches may play a role in future health risks, and researchers are starting to connect the dots regarding data in this area.
A
The results of the study showed that participants on GLP-1RAs saw a significant risk reduction for 10 out of 13 obesity-associated cancers compared to participants taking insulin.
The results suggest that GLP-1RAs may help prevent some obesity-associated cancers.
Having obesity or overweight can increase the risk for certain conditions. For example, having
Wael Harb, MD, board-certified hematologist and medical oncologist at MemorialCare Cancer Institute at Orange Coast and Saddleback Medical Centers in Orange County, CA, who was not involved in the study, explained how oebsity is connected to cancer to Medical News Today:
“Obesity is a well-established risk factor for several types of cancer. The mechanisms linking obesity to cancer involve chronic inflammation, insulin resistance, increased levels of insulin and insulin-like growth factors, altered levels of sex hormones, and adipokines. These factors can promote tumor development and progression.”
“Excess body fat also affects the body’s immune response and can create an environment conducive to cancer growth. Specific cancers associated with obesity include colorectal, breast, endometrial, kidney, and pancreatic cancers, among others.”
— Wael Harb, MD
Doctors can help address people’s risk for obesity-associated cancers, including discussing ways people can follow healthy diets and increase physical activity to maintain a healthy weight. It can also involve appropriate cancer screening for people who are more at risk for obesity-associated cancers.
Researchers are also interested in what tools and interventions could help people who are more at risk for obesity-associated cancers. The authors of the current study wanted to see how treatment interventions related to type 2 diabetes affected the risk for obesity-associated cancers.
This study was a retrospective observational study. To gather information from a large sample, researchers looked at deindentified electronic health records. They included data from over 1.6 million people in their analysis.
All participants had type two diabetes and had no history of any of the noted thirteen obesity-associated cancers. All participants had also been prescribed one of three medication types to assist with diabetes management:
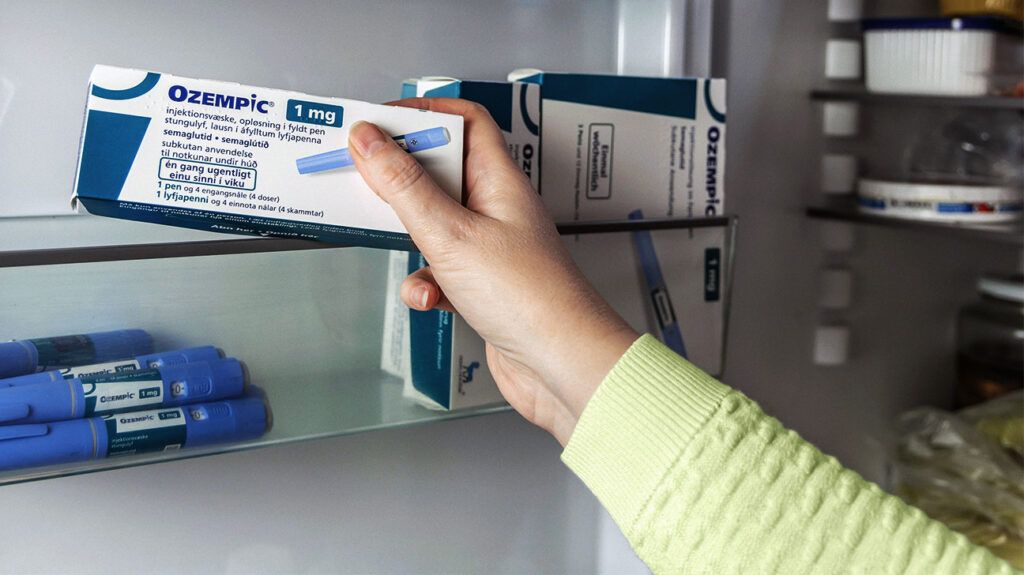
Glucagon-like peptide receptor agonists (GLP-1RAs) like Ozempic- Insulin
- Metformin
During the fifteen-year follow-up period, researchers examined the incidence of each of the thirteen obesity-associated cancers among participants. In their analysis, researchers found that participants prescribed GLP-1RAs had a lower associated risk for ten of the thirteen obesity-associated cancers than those prescribed insulin. This included a reduced risk for gallbladder, pancreatic, ovarian, colorectal, and esophageal cancer.
Risks related to stomach cancer in this comparison had a hazard ratio of less than one for participants who were taking GLP-1RAs compared to insulin users, but it did not reach a statistically significant level. The researchers did not find an association between GLP-RAs and a reduced risk for breast or thyroid cancer compared to insulin.
Next, researchers went on to compare risks for individuals on GLP-1RAs compared to those taking metformin. The risk for colorectal and gallbladder cancer for participants taking GLP-1RAs were reduced, but not statistically significant compared to those taking metformin.
Overall, researchers found that compared to metformin users, GLP-1RA users were not at a decreased risk for any of the cancers and were also at an increased risk for kidney cancer.
Harb noted the following clinical implications of the data:
“The potential clinical implications of these findings are significant. If GLP-1 RAs are indeed protective against certain obesity-related cancers, their use could be prioritized in the management of patients with T2D who are at high risk for these cancers. This could lead to a dual benefit of improved glycemic control and cancer risk reduction.”
“For example, the study showed that GLP-1RAs were associated with a hazard ratio of 0.35 for gallbladder cancer, 0.41 for pancreatic cancer, and 0.54 for colorectal cancer when compared to insulin, suggesting a substantial protective effect. Additionally, these findings may encourage further investigation into the mechanisms by which GLP-1 RAs exert these protective effects, potentially leading to the development of new therapeutic strategies,” he continued.
This study supports the idea that GLP-1RAs may help lower cancer risks. However, it is also important to consider the study’s limitations. First, because of the study’s nature and the use of electronic health records, there is a risk of diagnosis errors, confounding, and bias. Electronic health records also include data that is self-reported from participants, which can be inaccurate.
The study cannot prove cause and did not allow researchers to control for variables after participants’ first prescription. Researchers were also unable to identify individual patient data, which means they couldn’t do things like “correlate risk reduction with a degree of weight loss.” They also lacked data on medication adherence, which could have impacted the study’s findings. Finally, they could not explicitly control for participants’ insurance type and healthcare utilization.
Researchers note future research can confirm their results using other electronic health records databases and analytics. Further research is also needed to understand the potential risks for GLP-1RAs, such as a possible increase in risk for thyroid cancer.
Anton Bilchik, MD, PhD, surgical oncologist, chief of medicine, and Director of the Gastrointestinal and Hepatobiliary Program at Providence Saint John’s Cancer Institute in Santa Monica, CA, who was not involved in the study, offered the following words of caution regarding the study’s results as well:
“This study has reasonably long follow up and includes a large number of patients. While it shows a reduction in several obesity-related cancers, it remains unclear whether there is a direct effect of the GLP-1 drugs in preventing cancer or whether the reduction in cancer is related to weight loss as a result of the drug. This needs to be better elucidated.”
“The study further demonstrates how obesity increases the risk of several cancers and that exercise, nutrition and weight loss are important factors in reducing the risk. GLP-1 drugs are important as an adjunct to weight loss and therefore cancer prevention but should not be considered as a replacement for what we already know to be important in cancer risk reduction.”
— Anton Bilchik, MD, PhD
