Medicare Part B and Medicare Advantage cover medically necessary X-rays. However, there may be some out-of-pocket costs.
Medicare covers most medically necessary procedures, including X-rays. However, a person may need to pay additional costs out of pocket for each procedure.
The exact amount a person may need to pay can vary based on several factors, including whether they have met their deductible and their location.
Glossary of Medicare terms
We may use a few terms in this article that can be helpful to understand when selecting the best insurance plan:
- Out-of-pocket costs: An out-of-pocket cost is the amount a person must pay for medical care when Medicare does not pay the total cost or offer coverage. These costs can include deductibles, coinsurance, copayments, and premiums.
- Deductible: This is an annual amount a person must spend out of pocket within a certain period before an insurer starts to fund their treatments.
- Coinsurance: This is the percentage of treatment costs that a person must self-fund. For Medicare Part B, this is 20%.
- Copayment: This is a fixed dollar amount a person with insurance pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
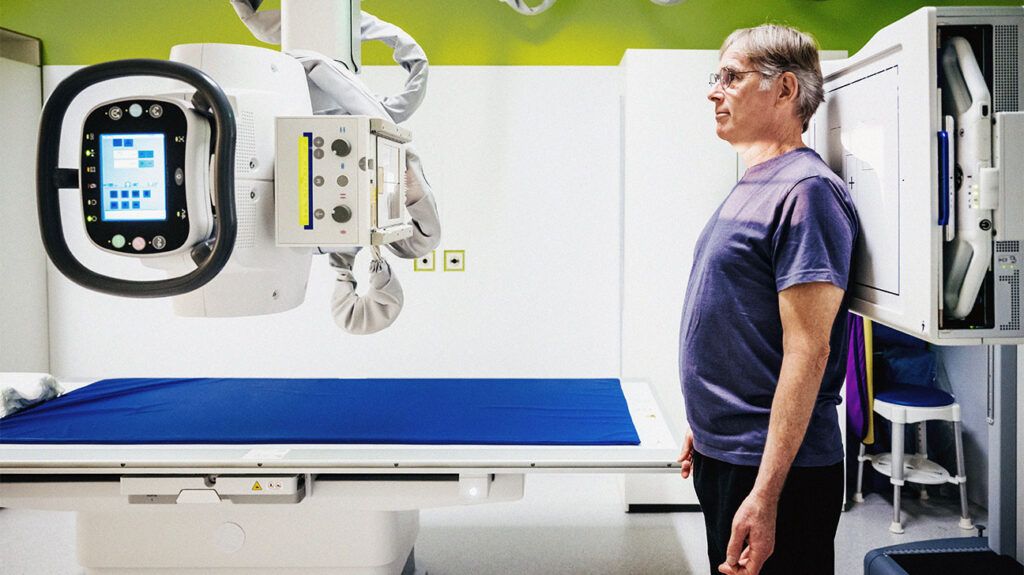
Medicare covers X-rays when a doctor or other qualified healthcare professional orders them for medically necessary diagnostic or treatment purposes.
X-rays may be done in a doctor’s office, healthcare facility, or hospital outpatient facility.
X-rays use electromagnetic radiation to generate images of structures inside the body. They can help doctors in the diagnosis of several health conditions. For example, X-rays allow doctors to:
- check for broken or fractured bones
- analyze the lungs for pneumonia
- look for foreign objects in the body
- examine masses or tumors
- look for calcifications
- examine certain types of injury to the body
Medicare also covers other diagnostic, non-laboratory tests, such as:
In order for Medicare to provide coverage, a doctor or facility needs to accept the assignment. This means they take Medicare insurance. The X-ray also needs to be for a medically necessary procedure.
People with Medicare Advantage (Part C) plans should also receive coverage for X-rays, though out-of-pocket costs may vary between providers.
Read about Original Medicare vs. Medicare Advantage.
Medicare Part B and Medicare Advantage (Part C) plans cover X-rays and other diagnostic assessments.
In order for Part B or Medicare Advantage to cover an X-ray, it must be deemed medically necessary.
According to Medicare, medically necessary refers to “services or supplies that meet accepted standards of medical practice to diagnose or treat your medical condition.”
If a doctor recommends an X-ray and Medicare denies the claim, a person can file an appeal. An appeal allows a person to contest the decision and gain coverage for the recommended X-ray or other service.
Read more about Medicare appeals.
The exact costs a person may pay for a Medicare-covered X-ray varies based on several factors.
Part B
Before a person meets the yearly deductible, a person will need to pay the amount up to the deductible before Medicare Part B will cover any of the cost of the X-ray.
In 2024, the annual Part B deductible is $240.
Once a person meets their deductible for the year, Part B will cover 80% of the cost of the X-ray. A person will then need to pay the remaining balance equal to 20% of the total cost of the X-ray.
Cost example
If a person has met their deductible for the year and the X-ray will cost $500, then the person will owe $100 (20% of $500).
If they have not met their deductible, they will owe $240 plus $52 (20% of $260) for a total cost of $292.
Medigap
Medigap is an optional insurance for people with Original Medicare (parts A and B). It can help cover the cost of X-rays. Medigap plans are optional plans that help cover costs a person will owe out of pocket, including:
- deductibles
- copayments
- coinsurance
Medigap also has a monthly premium that the person is responsible for paying.
Medicare Advantage
People with Medicare Advantage plans (Part C) may pay less out of pocket, depending on their plan. In general, the higher the monthly premium for a plan, the lower the deductible will be.
The plans also vary in how much of the costs they cover. Some plans may not require a copay or coinsurance payment. A person should contact their insurance provider to find out how much they will owe for X-rays and other services.
Other factors
Other factors can affect how much a person will owe for an X-ray whether they have Original Medicare or a Medicare Advantage plan. Some factors that affect price can include:
- whether the doctor accepts the assignment
- other insurance a person may have
- how much the doctor charges
- where a person gets an X-ray
- type of facility
Medicare resources
For more resources to help guide you through the complex world of medical insurance, visit our Medicare hub.
Medicare Part B and Medicare Advantage plans cover X-rays. A person will typically need to meet their deductible before Part B pays for some of the costs. Once a deductible is met, a person will owe 20% of the total cost of the X-ray.
A person may pay less out of pocket with a Medicare Advantage plan, though their monthly premium may be higher.
Medigap insurance can help cover the cost of an X-ray that Part B does not cover, but it will cost an additional monthly premium payment.
