CRVO occurs when blood can no longer travel through the main blood vessel that brings blood to the back of the eye. This can cause swelling, and it may lead to vision loss.
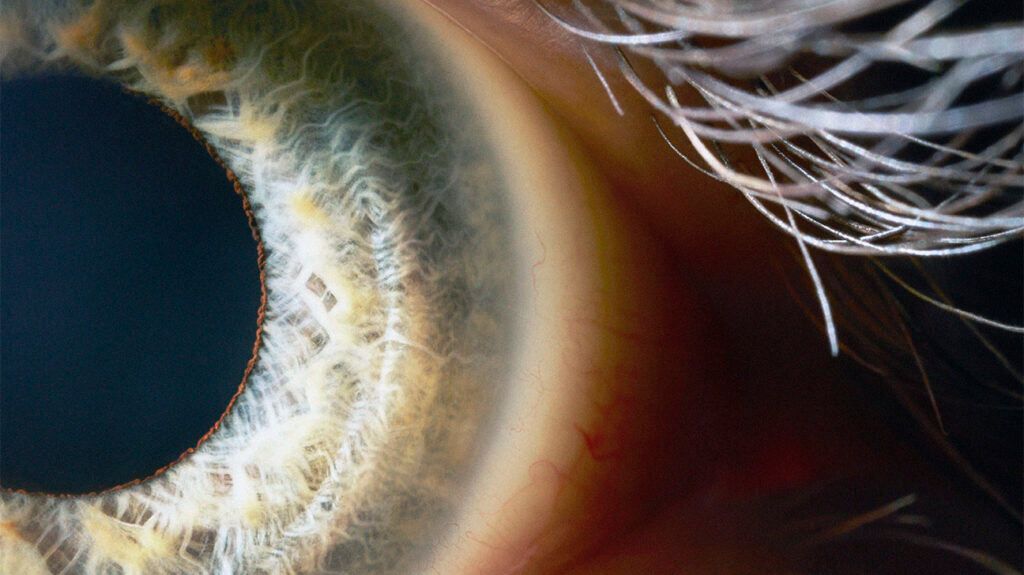
The retina is a layer of cells at the back of the eye that detects light and transmits signals to the brain, allowing a person to see.
One artery brings blood to the retina, and one vein takes blood away. If the vein develops a blockage, this can lead to blood leaking and swelling in the retina.
Read on to learn more about CRVO. This article looks at the symptoms and causes of the condition, risk factors, treatment options, and more.
CRVO most often causes mild symptoms. Sometimes, it
Some people with severe CRVO may experience:
- pressure
- redness in the eye
- floaters, or dark lines, wavy shapes, or spots that form due to small blood clumps leaking from the retina and moving across the eye
- blurry vision in part of the eye or the whole field of vision, which often occurs in the macula, or the center of the retina
- gradual vision loss
The direct cause of CRVO is unclear. However, it develops when something causes blood clots to block the central retinal vein, or when blood cannot flow through the vein as easily.
According to the American Society of Retina Specialists, CRVO most often develops in a single eye. If a doctor finds it in both, this may point to an underlying condition that increases blood clotting.
Two different types of CRVO can develop: Ischemic CRVO and nonischemic CRVO. They vary in severity and the way they reduce blood flow behind the eye.
Ischemic CRVO
Ischemic CRVO causes closed-off small blood vessels in the retina. The eye may be more likely to develop new small blood vessels, which increases the risk of bleeding in the retina.
If they develop in the front of the eye, eye fluids may not leave the eye as easily. As a result, glaucoma may develop due to increased eye pressure.
Usually, ischemic CRVO is the more severe of the two types. It causes worse vision problems than nonischemic CRVO and it is less likely that vision will improve.
Nonischemic CRVO
Nonischemic CRVO occurs when leaky blood vessels cause swelling in the macula.
It is the milder and more common type, occurring in around
Although the condition can be mild, treatment and monitoring may help individuals with nonischemic CRVO prevent it from becoming ischemic and more severe.
- glaucoma
- giant cell arteritis
- arteriosclerosis
- diabetes
- high blood pressure (hypertension)
- syphilis
- sarcoidosis
- HIV
- vasculitis
- migraine
- systemic conditions that increase blood clotting, such as:
- activated protein C resistance
- antiphospholipid syndrome
- Leiden factor V
- protein C and S deficiency
- hyperhomocysteinemia
- Waldenström’s disease
Other factors that make CRVO more likely to develop include:
- being over 50 years of age
- having a history of smoking
- being African American
- taking certain medications, including diuretics and oral contraceptives
If a person has symptoms of CRVO, an ophthalmologist, or eye doctor, may carry out a test known as fluorescein angiography. This involves injecting a dye into a vein elsewhere in the body, often in the arm. This dye travels through the blood vessels.
Using a specialized camera, the doctor can identify whether the dye travels through the central retinal vein. If it does not, the doctor may diagnose CRVO. They may also use optical coherence tomography (OCT) angiography, which involves checking retinal swelling without a dye using a special camera.
An ophthalmologist may recommend that people under the age of 40 years who show CRVO symptoms seek further testing for conditions that affect blood clotting.
In some people, CRVO resolves without treatment. This is the case for around one-third of older adults who do not receive treatment.
When treatment is necessary to prevent complications such as vision loss, several treatment options are available. These include:
- Anti-vascular endothelial growth factor (VEGF) injections: Anti-VEGF injections are the most common CRVO treatment. A doctor injects them straight into the eye to help reduce swelling.
- Steroid medication: This is another eye injection that may help bring down swelling. The effects of these medications often last for several months.
- Laser surgery: A type of laser surgery — panretinal photocoagulation — may reduce bleeding in the retina and resolve the increase in eye pressure. An ophthalmologist uses a laser to make small burns on the back of the retina. This treatment is usually more permanent than other types.
Vision usually takes a few months to improve after treatment. However, people with severe CRVO may not find that vision improves. A person’s eye doctor can provide them with more information about how effective treatment may be for CRVO.
How serious is central retinal vein occlusion?
Nonischemic CRVO, the
What is the life expectancy of a person with retinal occlusion?
A
Is retinal vein occlusion an eye stroke?
Some people refer to retinal vein occlusion as an “eye stroke,” as both retinal vein occlusion and strokes occur due to blocked or leaking blood vessels. However, an eye stroke is not the same as a stroke, where something reduces or stops the blood supply from reaching the brain.
Central retinal vein occlusion (CRVO) occurs when blood clots block the central retinal vein in the eye or blood leaks from the vessel, causing macular swelling. There are two types of CRVO: ischemic CRVO and nonischemic CRVO.
The condition has links to glaucoma, high blood pressure, diabetes, and arteriosclerosis, as well as conditions that increase blood clotting.
Some people do not experience symptoms, and the condition may resolve without treatment. However, for others, symptoms can include pressure, floaters, and vision problems. Treatment may be necessary to prevent the condition from worsening.
Treatment may include eye injections of anti-VEGF medications or steroids. In severe cases, laser surgery can help.
