Boniva is a brand-name prescription drug that’s used for osteoporosis after menopause. (Osteoporosis is a condition that causes weak and brittle bones.) Boniva comes in two forms:
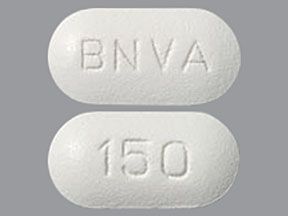
- Boniva tablets. The tablets are FDA-approved to prevent and treat osteoporosis.
- Boniva injections. The injections are FDA-approved to treat osteoporosis.
Both Boniva tablets and Boniva injections have certain limitations of use. For more information, see the “Boniva uses” section below.
Drug details
Boniva contains the active drug ibandronate and belongs to a group of drugs called bisphosphonates. Boniva works by slowing the breakdown of bone in your body. The medication also helps increase the amount of tissue in your bones, making them thicker and stronger.
Boniva tablets are swallowed and are available in one strength: 150 milligrams (mg). You’ll likely take Boniva tablets once per month.
If you’re not able to swallow Boniva tablets, your doctor may decide that Boniva injections are a better option for you. The injection is given as an intravenous (IV) infusion, which is an injection into a vein that’s given over a period of time. A healthcare professional will give you the injections in a doctor’s office, a clinic, or your home. Boniva injections are available in one strength: 3 mg/3 milliliters (mL).
Effectiveness
For information on the effectiveness of Boniva, see the “Boniva uses” section below.
The Food and Drug Administration (FDA) approves prescription drugs such as Boniva to prevent and treat certain conditions.
Boniva for preventing osteoporosis after menopause
Boniva tablets are FDA-approved to prevent osteoporosis after menopause.* (Boniva tablets and injections are also FDA-approved to treat osteoporosis after menopause. To learn more, see the “Boniva for treating osteoporosis after menopause” section below.)
Clinical studies of Boniva tablets haven’t lasted longer than 3 years. If your risk for having fractures is low while taking Boniva, your doctor will probably have you take the drug for 3 to 5 years. You can talk with them about how long you’ll likely use the medication.
* It isn’t known exactly how long you should take Boniva for this purpose. The amount of time you take the drug depends on your risk for developing fractures. (For more information, see the “Boniva side effects” section above.)
Osteoporosis explained
Osteoporosis is a condition that causes weak and brittle bones. It happens when your body isn’t able to make new bone as quickly as it loses old bone.
Osteoporosis is more likely to occur as you get older. During menopause, lower levels of sex hormones (such as estrogen) can increase your risk for osteoporosis. The condition can also be caused by other medications, such as corticosteroids.
Osteoporosis is usually discovered in a bone mineral density (BMD) test. (This is a test that measures the strength of your bones.) You may not have any symptoms of osteoporosis unless you’ve had it for a while. Osteoporosis may cause your height to decrease. The condition may also cause you to have a bent-over posture. Your bones may also break more easily than usual.
Effectiveness for preventing osteoporosis after menopause
Clinical studies have found Boniva tablets to be effective in preventing osteoporosis in women after menopause.
In these studies, Boniva tablets were compared with a placebo (a treatment without an active drug). Researchers wanted to know which treatment was better at improving the results of a BMD test for the spine.
After 2 years of treatment, women who were given Boniva tablets had stronger spinal bones. The average spine BMD results were 3.1% to 4.12% better for women given Boniva than for those given a placebo. (The percentages varied depending on the dose of Boniva tablets being studied.)
Boniva for treating osteoporosis after menopause
Boniva tablets and injections are FDA-approved to treat osteoporosis* after menopause. If you’re not able to swallow Boniva tablets, your doctor may decide that Boniva injections are a better option for you. (For more information, see the “How to take Boniva” section below.)
Boniva tablets are also FDA-approved to prevent osteoporosis after menopause. (To learn more, see “Boniva for preventing osteoporosis after menopause” above.)
Note: It isn’t known exactly how long you should take Boniva for these purposes. The amount of time you take the drug depends on your risk for having fractures as a side effect. (For more information, see the “Boniva side effects” section above.)
Clinical studies of Boniva injections haven’t lasted longer than 1 year. If your risk for having fractures is low while taking Boniva, your doctor will probably have you take the drug for 3 to 5 years. You can talk with them about how long you’ll likely use the medication.
* To learn more about osteoporosis, see “Osteoporosis explained” in the “Boniva for preventing osteoporosis after menopause” section above.
Effectiveness for treating osteoporosis after menopause
Clinical studies have found Boniva tablets and Boniva injections effective for treating osteoporosis in women after menopause.
In these studies, Boniva tablets were compared with Boniva injections. Researchers wanted to know which treatment was better at improving results of a BMD test for the spine.
After 1 year, the results showed that the spine BMD of women given Boniva injections improved by 4.5%. In comparison, the spine BMD of women given Boniva tablets improved by 3.5%.
These studies also compared Boniva tablets with a placebo (a treatment without an active drug). Researchers wanted to know which treatment was better at preventing new or worsening spine fractures.
Over 3 years of treatment, the results showed that:
- 4.7% of women given Boniva tablets had a new spine fracture
- 9.6% of women given a placebo had a new spine fracture
- 5.1% of women given Boniva tablets had a worsening spine fracture
- 10.4% of women given a placebo had a worsening spine fracture
Boniva and children
Boniva isn’t approved for use in children. It isn’t known if the drug is safe or effective for children.
Boniva is a brand-name drug that contains the active drug ibandronate. This active drug is also available as a generic medication. A generic drug is an exact copy of the active drug in a brand-name medication.
The generic is considered to be as safe and effective as the original drug. Generics tend to cost less than brand-name drugs.
If you’re interested in using the generic form of Boniva, talk with your doctor. They can tell you if it comes in forms and strengths that can be used for your condition.
Boniva can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Boniva. These lists don’t include all possible side effects. The side effects you experience may vary depending on the form of Boniva you take.
For more information on the possible side effects of Boniva, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Boniva, you can do so through MedWatch.
Mild side effects
Mild side effects of Boniva can include:*
- abdominal (belly) pain
- arm or leg pain
- diarrhea
- constipation
- nausea
- indigestion (upset stomach)
- flu-like symptoms, such as fever, chills, or fatigue (lack of energy)
- bronchitis (a type of lung infection)
- headache
- hypertension (high blood pressure)
- back pain†
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
* This is a partial list of mild side effects from Boniva. To learn about other mild side effects, talk with your doctor or pharmacist. You can also refer to the Medication Guide for the form of Boniva you’re using: Boniva tablet or Boniva injection.
† For more information on this side effect, see the “Side effect details” section below.
Serious side effects
Serious side effects from Boniva aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Esophagus problems, such as ulcers, inflammation, narrowing, or wearing away of the esophagus. (The esophagus is the tube that connects your mouth to your stomach.) Symptoms can include:
- loss of appetite
- pain when swallowing
- trouble swallowing
- Low level of calcium. Symptoms can include:
- fatigue (lack of energy)
- feeling of pins and needles in the arms or legs
- memory problems
- muscle spasms (cramps) or stiffness
- Kidney problems, such as acute renal failure. Symptoms can include:
- confusion
- dark-colored urine
- leg swelling
- nausea
- urinating a smaller amount than usual
- Allergic reaction.*
- Jaw and dental problems.*
- Bone, joint, and muscle pain.*
- Thigh fracture.*
* For more information on this side effect, see “Side effect details” below.
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here’s some detail on certain side effects this drug may or may not cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Boniva. Clinical studies looked at women who had gone through menopause. Researchers found that 3% of the women who took Boniva tablets had an allergic reaction. In comparison, 2% of the women in these studies who took a placebo had an allergic reaction. (A placebo is a treatment without an active drug.)
It isn’t known how many may have had an allergic reaction in clinical studies of Boniva injections.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Boniva. Call 911 or your local emergency number if your symptoms feel life threatening or if you think you’re having a medical emergency.
Jaw and dental problems
Boniva can cause a jaw problem known as osteonecrosis, which occurs when the jawbone doesn’t have enough blood flow. It isn’t known how many people may have had jaw problems in clinical studies of Boniva tablets or Boniva injections.
Jaw problems can occur suddenly after you start to use Boniva. Your risk for having jaw or dental problems while using Boniva may increase as you keep using the drug. Your risk may also be higher if you:
- have anemia (low level of red blood cells)
- have cancer
- have certain dental problems, such as dentures that fit poorly
- have had a dental procedure, such as a tooth removal or dental implants
- have poor oral health
- take chemotherapy, a corticosteroid, or an angiogenesis inhibitor (a type of cancer drug)
Symptoms of osteonecrosis can include:
- loose teeth
- mouth sores
- jaw pain or discomfort
- slow healing of the affected area after dental surgery or after a tooth is pulled
If you’re using Boniva, be sure to tell your doctor if you plan to have dental surgery or any teeth removed. Also, before having any dental work, you should tell your dentist if you’re taking Boniva. Your doctor or dentist may have you stop taking Boniva for a time to lower your risk for the side effects mentioned above.
Bone, joint, and muscle pain
Bone, joint, and muscle pain may occur with Boniva use. In clinical studies, women who had gone through menopause were given Boniva tablets, Boniva injections, or a placebo.
In these studies, bone, joint, or muscle pain occurred in:
- 0.8% to 10% of women taking Boniva
- 3% to 5% of women taking a placebo
The percentages varied depending on the form or dose of Boniva being studied.
Bone, joint, and muscle pain can occur as soon as a day after you start taking Boniva. Or they could occur several months after you start using the medication. It’s not known how long the pain lasted in the clinical studies.
While using Boniva, tell your doctor if you have bone, joint, or muscle pain that bothers you. They may perform tests to see whether the pain is a sign of a more serious side effect, such as a thigh fracture. (For more information about this side effect, see “Thigh fracture” below.)
Back pain
Back pain is a possible side effect of Boniva. In clinical studies, women who had gone through menopause received Boniva tablets, Boniva injections, or a placebo.
In these studies, back pain occurred in:
- 4.3% to 14% of women taking Boniva
- 12% of women taking a placebo
The percentages varied depending on the form or dose of Boniva being studied.
If you’re bothered by back pain while using Boniva, tell your doctor. They may recommend a different medication for you.
Thigh fracture
A fracture of the thigh bone is possible with Boniva use. It’s not known how many people may have had thigh fractures in clinical studies of Boniva tablets or Boniva injections.
This type of fracture can happen in either leg and can occur with only light force to the thigh bone. You may have pain in your thigh area for several weeks before the fracture occurs. Your risk for having a fracture in your thigh while taking Boniva may increase if you’re using corticosteroids. (Corticosteroids are a type of drug used to reduce inflammation.)
If you have thigh pain while taking Boniva, tell your doctor right away. They’ll likely perform tests to see whether you have a fracture.
Weight gain (not a side effect)
Weight gain wasn’t a reported side effect in clinical studies of Boniva tablets or Boniva injections. However, weight gain is a known side effect of similar drugs, such as Fosamax. (For more information about Fosamax, see the “Boniva vs. Fosamax” section below.)
Weight gain is also common during menopause. This can happen because of age, genetics, lifestyle, or hormone changes. Since Boniva is used after menopause, it’s possible that you may gain weight after you start taking it. However, it’s not likely that the drug would be the cause of the weight gain.
If you’re concerned about weight gain while taking Boniva, talk with your doctor. They can recommend healthy ways for you to manage your weight while taking this drug.
How long do side effects of Boniva last?
The amount of time that side effects last after you take Boniva can vary. For example, after your first Boniva dose, you may have flu-like symptoms that usually go away within 48 hours. However, bone, joint, or muscle pain may last for several weeks, especially if the pain is a sign of a possible thigh fracture.
Be sure to tell your doctor about any possible side effects you experience while taking Boniva. They can help determine whether these side effects are serious. Your doctor can also help you decide if a different drug option is better for you.
The Boniva dosage your doctor prescribes will depend on several factors. These include:
- the form of Boniva you take
- other medical conditions you may have
Your doctor will start you on the typical Boniva dosage used to prevent or treat osteoporosis. Then they’ll check your condition on a regular basis to decide if you need to keep taking the drug. Your doctor will ultimately prescribe Boniva for the shortest amount of time needed to prevent or treat osteoporosis. The goal is to help lower your risk for side effects. (For information on side effects, see the “Boniva side effects” section above.)
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Boniva comes in two forms:
- Tablet. Boniva tablets are swallowed and are available in one strength: 150 milligrams (mg).
- Injection. If you’re not able to swallow Boniva tablets, your doctor may decide that Boniva injections are a better option for you. The injection is given as an intravenous (IV) infusion for 15 to 30 seconds. An infusion is an injection into a vein that’s given over a period of time. A healthcare professional will give you the injections in a doctor’s office, a clinic, or your home. Boniva injections are available in one strength: 3 mg/3 milliliters (mL).
Boniva tablet dosage for preventing and treating osteoporosis after menopause
Boniva tablets are approved to prevent and treat osteoporosis after menopause. In both cases, the typical dosage of Boniva is one 150-mg tablet, once a month. It should be taken on the same day each month. (This is sometimes referred to as your “Boniva day.”)
For important information about how to take each dose of Boniva tablets, see the “How to take Boniva” section below.
Boniva injection dosage for treating osteoporosis after menopause
Boniva injections are approved to treat osteoporosis after menopause. If you’re not able to swallow Boniva tablets, your doctor may decide that Boniva injections are a better option for you.
The typical dosage is one 3-mg injection, once every 3 months.
The injection is given as an intravenous (IV) infusion. To learn more, see “Drug forms and strengths” above.
What if I miss a dose?
If you miss a dose of a Boniva tablet, take your missed dose as soon as you remember. If it’s 7 days or sooner until your next dose, skip your missed dose. Then take your next dose on the day of the month you typically take Boniva.
You shouldn’t double up on doses to make up for your missed dose. This can raise your risk for having side effects from Boniva. (For more information on side effects, see the “Boniva side effects” section above.)
If you miss an appointment for a Boniva injection, call your doctor’s office to reschedule as soon as possible.
To help make sure that you don’t miss a dose, try using a medication reminder. This can include setting an alarm on your phone or downloading a reminder app. It may also be helpful to put your dosage schedule on a calendar.
Will I need to use this drug long term?
The amount of time you’ll take Boniva depends on your risk for developing fractures. If your risk is low, your doctor typically will have you stop using Boniva after 3 to 5 years. (For more information about this, see the “Boniva uses” section below.)
If you have questions about the amount of time that it’s safe for you to take Boniva, talk with your doctor.
You may wonder how Boniva compares with other medications that are prescribed for similar uses. Here we look at how Boniva and Fosamax are alike and different.
Ingredients
Boniva contains the active drug ibandronate. Fosamax contains the active drug alendronate.
Both Boniva and Fosamax belong to a group of drugs called bisphosphonates. Boniva and Fosamax work by slowing the breakdown of bone in your body.
Uses
Here is a list of conditions that the Food and Drug Administration (FDA) has approved Boniva and Fosamax to be used for:
- Both Boniva* and Fosamax are FDA-approved to:
- Prevent or treat osteoporosis after menopause. (Osteoporosis is a condition that causes weak and brittle bones.)
- Fosamax is also FDA-approved to:
- Increase bone mass in people who have osteoporosis.
- Treat osteoporosis caused by corticosteroids.
- Treat Paget’s disease.
* Boniva has certain limitations of use. For more information, see the “Boniva uses” section below.
Drug forms and administration
Boniva comes in two forms:
- Boniva tablets. The tablets are approved to prevent and treat osteoporosis. Boniva tablets are swallowed and typically taken once per month.
- Boniva injections. The injections are approved to treat osteoporosis. They may be an option if you’re not able to swallow Boniva tablets. Each injection is given as an intravenous (IV) infusion, which is an injection into a vein that’s given over a period of time. A healthcare professional will give you the injections in a doctor’s office, a clinic, or your home.
Fosamax comes as a tablet that you swallow. You may take Fosamax once per day or once per week.
Side effects and risks
Boniva and Fosamax both prevent or treat osteoporosis. Therefore, these medications can cause very similar side effects, but some different ones as well. Below are examples of these side effects.
Mild side effects
These lists contain up to 10 of the most common mild side effects that can occur with each drug, as well as common side effects that both drugs may share.
- Can occur with Boniva:
- arm or leg pain
- Can occur with Fosamax:
- hair loss
- Can occur with both Boniva and Fosamax:
- abdominal (belly) pain
- indigestion (upset stomach)
- nausea
Serious side effects
These lists contain examples of serious side effects that can occur with Boniva or that both Boniva and Fosamax share.
- Can occur with Boniva:
- kidney problems, such as acute renal failure
- Can occur with Fosamax:
- no unique serious side effects
- Can occur with both Boniva and Fosamax:
- esophagus problems, such as ulcers, inflammation, narrowing, or wearing away of the esophagus
- bone, joint, and muscle pain
- jaw and dental problems, such as osteonecrosis
- low level of calcium in the blood
- thigh fracture
Effectiveness
Boniva and Fosamax have different FDA-approved uses, but they’re both used to prevent or treat osteoporosis after menopause.
The use of Boniva and Fosamax in treating osteoporosis after menopause has been directly compared in a
Costs
The costs of Boniva tablets and Fosamax tablets may vary depending on your treatment plan. The actual price you’ll pay for either drug depends on your treatment plan, your insurance, your location, and the pharmacy you use. For Boniva injections, it will also depend on the cost of the visit to your healthcare professional to receive your doses.
Boniva and Fosamax are both brand-name drugs. Boniva is also available as a generic drug called ibandronate. Fosamax is available as a generic drug called alendronate. A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. Generics tend to cost less than brand-name drugs.
Like Fosamax (above), the drug Prolia has uses similar to those of Boniva. Here’s a comparison of how Boniva and Prolia are alike and different.
Ingredients
Boniva contains the active drug ibandronate. Prolia contains the active drug denosumab.
Boniva belongs to a class of drugs called bisphosphonates. (A class of drugs is a group of medications that work in a similar way.)
Prolia belongs to a class of drugs called monoclonal antibodies.
Even though they’re in different drug classes, Boniva and Prolia both work by slowing the breakdown of bone in your body.
Uses
Here’s a list of conditions that the Food and Drug Administration (FDA) has approved Boniva* and Prolia to be used for:
- Both Boniva and Prolia are FDA-approved to:
- Treat osteoporosis after menopause. (Osteoporosis is a condition that causes weak or brittle bones.) Prolia is specifically for use in those who have a high risk for fractures.
- Boniva is also FDA-approved to:
- Prevent osteoporosis after menopause.
- Prolia is also FDA-approved for the following uses in people at high risk for fractures:
- Increase bone mass in men with osteoporosis.
- Treat osteoporosis caused by corticosteroids.
- Increase bone mass in people who are taking certain breast cancer drugs that lower estrogen levels.
- Increase bone mass in those with nonmetastatic prostate cancer who are taking drugs to lower the level of male hormones.
* Boniva has certain limitations of use. For more information, see the “Boniva uses” section below.
Drug forms and administration
Boniva comes in two forms:
- Boniva tablets. The tablets are approved to prevent and treat osteoporosis. Boniva tablets are swallowed and typically taken once per month.
- Boniva injections. The injections are approved to treat osteoporosis. They may be an option if you’re not able to swallow Boniva tablets. Each injection is given as an intravenous infusion, which is an injection into a vein that’s given over a period of time. A healthcare professional will give you the injections in a doctor’s office, a clinic, or your home.
Prolia is given as a subcutaneous injection (an injection under the skin) by a healthcare professional. The drug is typically given once every 6 months.
Side effects and risks
Boniva and Prolia both treat osteoporosis. Therefore, these medications can cause very similar side effects, as well as some different ones. Below are examples of these side effects.
Mild side effects
These lists contain up to 10 of the most common mild side effects that can occur with each drug, as well as mild side effects that both drugs may share.
- Can occur with Boniva:
- indigestion (upset stomach)
- Can occur with Prolia:
- swelling of the arms or legs
- Can occur with both Boniva and Prolia:
- abdominal (belly) pain
- arm, leg, and back pain
- hypertension (high blood pressure)
- bronchitis (a type of lung infection)
Serious side effects
These lists contain examples of serious side effects that can occur with Boniva or Prolia, as well as serious side effects that both drugs may share.
- Can occur with Boniva:
- esophagus problems, such as ulcers, inflammation, narrowing, or wearing away of the esophagus
- kidney problems, such as acute renal failure
- Can occur with Prolia:
- spine fractures when Prolia treatment is stopped
- Can occur with both Boniva and Prolia:
- bone, joint, and muscle pain
- jaw and dental problems, such as osteonecrosis
- low level of calcium in the blood
- thigh fracture
Effectiveness
Boniva and Prolia have different FDA-approved uses. However, they’re both used to treat osteoporosis after menopause.
The use of Boniva and Prolia in treating osteoporosis after menopause has been directly compared in a clinical study. One group of women was given Boniva once per month. The other group was given Prolia once every 6 months. After 1 year of treatment, the researchers found Prolia to be more effective at increasing bone strength than Boniva.
Costs
The cost of Boniva and Prolia may vary depending on your treatment plan. The actual price you’ll pay for either drug also depends on your insurance plan, your location, and the pharmacy you use. In addition, for Boniva and Prolia injections, the price will depend on the cost of the visit to your healthcare professional to receive your doses.
Boniva and Prolia are both brand-name drugs. Boniva is also available as a generic drug called ibandronate. There are currently no generic forms of Prolia. Brand-name medications usually cost more than generics.
Other drugs are available that can prevent or treat osteoporosis after menopause. Some may be a better fit for you than others. If you’re interested in finding an alternative to Boniva, talk with your doctor. They can tell you about other medications that may work well for you.
Alternatives for preventing osteoporosis after menopause
Examples of other drugs that may be used to prevent osteoporosis after menopause include:
- alendronate (Fosamax)
- alendronate and vitamin D (Fosamax Plus D)
- conjugated estrogens (Premarin)
- estrogen/medroxyprogesterone (Premphase, Prempro)
- raloxifene (Evista)
- risedronate (Actonel)
- zoledronic acid (Reclast)
Alternatives for treating osteoporosis after menopause
Examples of other drugs that may be used to treat osteoporosis after menopause include:
- abaloparatide (Tymlos)
- alendronate (Fosamax)
- calcitonin (Miacalcin)
- denosumab (Prolia)
- raloxifene (Evista)
- risedronate (Actonel)
- romosozumab (Evenity)
- teriparatide (Forteo)
- zoledronic acid (Reclast)
As with all medications, the cost of Boniva can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Boniva injections from a healthcare professional. This form of Boniva isn’t typically available at a pharmacy. You’ll need help from a healthcare professional to receive Boniva injections safely and effectively. The cost of Boniva injections also depends on the cost of the visits to your healthcare professional to receive each dose.
Before approving coverage for Boniva, your insurance company may require you to get prior authorization. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the prior authorization request and decide if the drug will be covered.
If you’re not sure if you’ll need to get prior authorization for Boniva, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Boniva, or if you need help understanding your insurance coverage, help is available.
Genentech, the manufacturer of Boniva, offers a patient resource center. For more information and to find out if you’re eligible for support, call 877-GENENTECH (877-436-3683).
Generic version
Boniva is available in a generic form called ibandronate. A generic drug is an exact copy of the active drug in a brand-name medication. The generic is considered to be as safe and effective as the original drug. And generics tend to cost less than brand-name drugs.
If your doctor has prescribed Boniva and you’re interested in using ibandronate instead, talk with your doctor. They may have a preference for one version or the other. You’ll also need to check your insurance plan, as it may only cover one or the other.
You should take Boniva according to your doctor’s or healthcare professional’s instructions.
Boniva comes in two forms. One is a tablet that you swallow. The other form is an injection. The injection is given as an intravenous infusion for 15 to 30 seconds. An infusion is an injection into a vein that’s given over a period of time. A healthcare professional will give you the injections in a doctor’s office, a clinic, or your home.
When to take
Below is information about when to take Boniva, depending on whether you use the tablet or injection form.
Boniva tablets
You should avoid eating or drinking anything (other than plain water) at least 1 hour before taking Boniva.
Boniva tablets should be taken in the morning with at least 6 ounces (oz) to 8 oz of plain water. You shouldn’t use water that contains vitamins or supplements, such as mineral water. This is because these types of water may contain high levels of calcium, which can make Boniva less effective. (For more information, see the “Boniva interactions” section below.)
You should take Boniva tablets while standing or sitting up. After taking the drug, don’t lie down for at least 60 minutes. This is because the Boniva tablet can cause problems with your throat if the tablet remains there for too long.
Standing or sitting up helps make sure the tablet is swallowed completely and moves out of your esophagus. This lessens your risk for having esophagus problems, such as ulcers or inflammation. (For more information on this side effect, see the “Boniva side effects” section above.)
After taking Boniva, you should wait at least 1 hour to eat or drink anything (other than plain water).
Boniva injections
If you’re not able to swallow Boniva tablets, your doctor may decide that Boniva injections are a better option for you. Boniva injections are given by a healthcare professional once every 3 months.
Drug reminders
To help make sure that you don’t miss a dose of Boniva tablets or an appointment for a Boniva injection, try using a medication reminder. This can include setting an alarm on your phone or downloading a reminder app. It may also be helpful to put your dosage schedule on a calendar.
Taking Boniva with food
You should take Boniva tablets on an empty stomach. You should avoid eating or drinking anything (other than plain water) at least 1 hour before and 1 hour after taking Boniva.
You shouldn’t use water that contains vitamins or supplements, such as mineral water. This is because these types of water may contain high levels of calcium, which can make Boniva less effective. (For more information, see the “Boniva interactions” section below.)
Taking Boniva with food can decrease the amount of the drug that your body absorbs. This could make Boniva less effective for your condition.
Can Boniva tablets be crushed, split, chewed, or sucked?
No, you shouldn’t crush, split, chew, or suck Boniva tablets. You should always swallow them whole. If you crush, split, chew, or suck on Boniva tablets, you may raise your risk for esophagus problems, such as ulcers or inflammation. The esophagus is the tube from your mouth to your stomach. (For more information on this side effect, see the “Boniva side effects” section above.)
If you have trouble swallowing Boniva tablets, tell your doctor. They may suggest that you try Boniva injections instead.
Boniva is FDA-approved to treat and prevent osteoporosis after menopause.
What happens with osteoporosis
Osteoporosis is a condition that causes weak and brittle bones. It happens when your body isn’t able to make new bone as quickly as it loses old bone. Osteoporosis is more likely to occur as you get older.
During menopause, lower levels of sex hormones (such as estrogen) can increase your risk for osteoporosis. The condition can also be caused by other medications, such as corticosteroids.
What Boniva does
Boniva belongs to a group of drugs called bisphosphonates. Boniva works to help prevent and treat osteoporosis by slowing the breakdown of bone in your body. Boniva also helps increase the amount of tissue in your bones. This helps make your bones thicker and stronger.
How long does it take to work?
Boniva begins working right away to prevent or treat osteoporosis. But you probably won’t notice Boniva acting in your body. This is because Boniva works over time to prevent or stop your bones from breaking down.
To make sure Boniva is working for you, your doctor will probably check your bone mineral density (BMD). It might take about 6 months for the BMD test to show improvements in your bone strength.
How long does Boniva stay in your system?
The amount of time Boniva stays in your system can vary depending on whether you take the tablet or injection form of the drug. Each form should keep working in your body until it’s time to receive your next dose. Each Boniva tablet dose should stay in your system for about 1 month. And each dose of a Boniva injection should stay in your system for about 3 months.
For information about how long side effects may last after you stop taking Boniva, see “How long do side effects of Boniva last?” in the “Boniva side effects” section above.
Here are answers to some frequently asked questions about Boniva.
How long is Boniva safe to take?
It isn’t known exactly how long it’s safe to take Boniva. The amount of time you take the drug depends on your risk for developing fractures. If your risk is low, your doctor will typically have you take Boniva for 3 to 5 years. If your risk is high, they may have you use the drug for a longer period of time.
If you have questions about the amount of time that it’s safe for you to take Boniva, talk with your doctor.
Does Boniva cause hair loss?
No, hair loss wasn’t a side effect reported in clinical studies of Boniva tablets or Boniva injections. (For information on side effects, see the “Boniva side effects” section above.)
However, hair loss can occur during menopause. And it’s a possible side effect of other drugs, such as conjugated estrogens/medroxyprogesterone (Prempro), that are used to treat menopause symptoms.
If you’re concerned about hair loss while using Boniva, talk with your doctor.
Can I use pain medication while taking Boniva?
Yes, if your doctor tells you that it’s safe, you can use pain medication while taking Boniva. However, taking Boniva tablets with aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) can increase your risk for an upset stomach. (Aspirin and other NSAIDs are used to treat pain.) For more information, see the “Boniva interactions” section below.
If you experience pain while taking Boniva, talk with your doctor. They can advise you on which treatments may help.
Do I need to take calcium and vitamin D supplements while using Boniva?
Yes, you may need to take calcium and vitamin D supplements with Boniva if your doctor recommends it. For more information, see the “Boniva use with other drugs” section below.
Why can’t I lie down right after taking Boniva tablets?
Lying down right after taking Boniva tablets can prevent you from swallowing the tablet completely. If this happens, Boniva may stay in your esophagus and lead to problems such as ulcers or inflammation. (For more information about this side effect, see the “Boniva side effects” section above.)
If you have questions about the best way to take Boniva tablets, see the “How to take Boniva” section above. You can also talk with your doctor or pharmacist.
Boniva can cause low calcium levels. If your level is already low, taking the drug could drop the level even further. Because of this, you should avoid taking Boniva if you have low calcium levels. (To learn more, see the “Boniva precautions” section below.)
Your doctor may give you a calcium test or a vitamin D test to see if you have low levels of calcium or vitamin D. If you do, they may recommend that you take calcium or vitamin D supplements while you are taking Boniva.
Boniva isn’t known to cause low levels of vitamin D. But vitamin D helps your body absorb calcium. For this reason, your doctor may check your vitamin D levels to make sure they are high enough to help absorb calcium. Even if you don’t have low vitamin D levels, your doctor will likely suggest that you still take vitamin D with calcium to help your body absorb the calcium.
If you take calcium and vitamin D supplements, be sure to take them at least 60 minutes after your Boniva tablet. (For more information, see the “Boniva interactions” section below.)
If you receive Boniva injections, they shouldn’t be mixed or given with liquid solutions or intravenous (IV) medications that contain calcium.
For any questions about taking calcium and vitamin D supplements while using Boniva, talk with your doctor.
To learn more about low calcium levels and other side effects, see the “Boniva side effects” section above.
There aren’t any known interactions between Boniva and alcohol. However, drinking heavy amounts of alcohol over many years can increase your risk for osteoporosis (weak and brittle bones). Menopause also increases your risk for osteoporosis. You may have a higher risk for osteoporosis if you’re going through menopause and have a history of heavy alcohol use.
Talk with your doctor about how much alcohol is safe for you to drink while taking Boniva.
Boniva can interact with several other medications. It can also interact with certain supplements as well as certain foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Boniva and other medications
Below is a list of medications that can interact with Boniva. This list doesn’t contain all drugs that may interact with Boniva.
Before taking Boniva, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Boniva tablets and certain drugs for heartburn or indigestion
Boniva tablets can interact with certain antacids and other medications used to help relieve heartburn or indigestion. Taking these medications with Boniva can make Boniva less effective. The medications include products that contain calcium, aluminum, magnesium, or iron.
Examples of these antacids and other medications that ease heartburn or indigestion include:
- Mylanta
- Gaviscon
- milk of magnesia
You should take antacids or drugs that contain calcium, aluminum, magnesium, or iron at least 1 hour after taking a Boniva tablet. This can help lessen your risk for the interaction.
If you have questions about using Boniva tablets with these medications, talk with your doctor.
Boniva tablets and nonsteroidal anti-inflammatory drugs
Taking Boniva tablets with nonsteroidal anti-inflammatory drugs (NSAIDs) can increase your risk for certain side effects. NSAIDs can cause an upset or irritated stomach. Taking Boniva tablets can also cause an upset stomach. Therefore, taking Boniva tablets while you’re also using NSAIDs can increase your risk for this side effect even more.
Examples of NSAIDs include:
Before you start using Boniva tablets, be sure to tell your doctor about all medications you take. This includes over-the-counter medications such as NSAIDs. If you take these drugs, your doctor may recommend a medication other than Boniva.
Boniva and herbs and supplements
Herbs or supplements that contain calcium or certain vitamins can interact with Boniva. (For more information, see the “Boniva tablets and certain drugs for heartburn or indigestion” section above.) Be sure to check with your doctor or pharmacist before using any of these products while taking Boniva.
Boniva and foods
You should avoid eating or drinking anything (other than plain water) at least 1 hour before and 1 hour after taking Boniva tablets.
You shouldn’t use water that contains vitamins or supplements, such as mineral water. This is because these types of water may contain high levels of calcium, which can make Boniva less effective.
Taking Boniva with food can decrease the amount of the drug that your body absorbs. This could make Boniva less effective for your condition.
No food interactions were reported with Boniva injections.
Boniva and lab tests
Bone and joint pain may occur with Boniva use. If you have bone or joint pain, your doctor may perform a bone scan. (This test can help your doctor see if you have a fracture or a more serious bone problem, such as bone cancer.)
During a bone scan, your doctor may inject a dye that helps your bones show up on the scan. Drugs from the bisphosphonate drug class,* such as Boniva tablets or injections, can make the dye less visible. As a result, it would be harder to see your bones on the scan. There have been no studies that looked at the effects of Boniva on bone scans.
If you plan to have a bone scan while taking Boniva tablets or receiving Boniva injections, talk with your doctor. They can advise you on when you should have your Boniva dose.
* A drug class is a group of medications that work in a similar way.
It isn’t known if Boniva is safe to take during pregnancy. The drug hasn’t been studied in pregnancy. Based on animal studies, Boniva tablets and Boniva injections harmed the fetus when the drugs were given during pregnancy. But animal studies don’t always predict what will happen in humans.
If you’re pregnant or planning a pregnancy, talk with your doctor. They can review the risks and benefits of using Boniva and whether a different medication is right for you.
Boniva and fertility
Based on animal studies, taking Boniva tablets may lead to fertility problems (trouble conceiving a child). Animal studies of Boniva injections have shown fertility problems for some women and men. However, animal studies don’t always predict what will happen in humans.
If you’re planning a pregnancy, talk with your doctor before using Boniva.
It’s not known if Boniva is safe to take during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while you’re using Boniva.
For more information about taking Boniva during pregnancy, see the “Boniva and pregnancy” section above.
It’s not known whether it’s safe to take Boniva while breastfeeding. This is because it isn’t known whether Boniva can pass into breast milk. The drug hasn’t been studied in people who are breastfeeding. Based on animal studies, Boniva tablets and Boniva injections may be able to pass into breast milk. But animal studies don’t always predict what happens in humans.
If you’re breastfeeding or planning to breastfeed, talk with your doctor before you use Boniva. They can advise you on the pros and cons of the drug and review prevention and treatment options other than Boniva.
This drug comes with several precautions.Before taking Boniva, talk with your doctor about your health history. Boniva may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Dental problems or upcoming dental procedures. Taking Boniva when you’ve had certain dental work can cause a jaw problem known as osteonecrosis. (For more information, see the “Boniva side effects” section above.) Be sure to tell your doctor if you plan to have dental surgery or any teeth removed while using Boniva. They may have you pause your Boniva use to lower your risk for osteonecrosis.
- Kidney disease. You shouldn’t take Boniva if you have kidney disease. Boniva can raise your risk for having kidney problems, which can make your kidney disease worse. Before you start using Boniva, tell your doctor if you have kidney disease. They may want to check your kidney function before you begin using Boniva. Your doctor may also recommend a medication other than Boniva.
- Low level of calcium. If you have a low calcium level, you shouldn’t take Boniva. Your doctor may recommend that you take calcium supplements before you start using Boniva. The drug can lower calcium levels, so your doctor may want to raise your level before you begin taking Boniva. If you have a low calcium level, talk with your doctor before you start taking Boniva. If you’re not sure about your calcium level, your doctor may test your blood.
- Low level of vitamin D. If your vitamin D level is low, your doctor may recommend that you take vitamin D supplements before you start using Boniva. This is because vitamin D helps your body absorb calcium. Your doctor may want to raise your vitamin D level before you take Boniva to help your body absorb more calcium. If you have a low vitamin D level, talk with your doctor before you start using Boniva. If you’re not sure about your vitamin D level, your doctor may test your blood.
- Esophagus problems. If you have problems with your esophagus, such as trouble swallowing, be sure to tell your doctor before using Boniva. The tablet form of the drug can increase your risk for esophagus problems. This is because the tablet could remain in your esophagus for a longer time than is safe. Therefore, esophagus problems could worsen while taking Boniva. Before using Boniva, talk with your doctor about any esophagus problems you may have. (For more information, see the “Boniva side effects” section above.)
- Problems absorbing nutrients. Tell your doctor if you have problems absorbing nutrients such as calcium. Not being able to properly absorb nutrients can be due to conditions such as celiac disease and lactose intolerance. If you have either of these conditions, you may have a higher risk for side effects from Boniva, such as a low calcium level. Before using Boniva, talk with your doctor about any problems you have absorbing nutrients. (For more information about side effects, see the “Boniva side effects” section above.)
- Allergic reaction. If you’ve had an allergic reaction to Boniva or any of its ingredients, you shouldn’t take Boniva. Ask your doctor what other medications are better options for you.
- Pregnancy. It’s not known if Boniva is safe to use during pregnancy. For more information, see the “Boniva and pregnancy” section above.
- Breastfeeding. It’s not known whether it’s safe to take Boniva while breastfeeding. For more information, see the “Boniva and breastfeeding” section above.
- Problems sitting up or standing for an extended time. After taking a Boniva tablet, you’ll need to sit up or stand for 1 hour. This helps reduce the risk of the tablet remaining in your esophagus for a longer time than is safe. If you’re not able to sit up or stand for 1 hour, talk with your doctor. They may recommend Boniva injections or a different medication. (To learn more about taking Boniva, see the “How to take Boniva” section above.)
Note: For more information about the potential negative effects of Boniva, see the “Boniva side effects” section above.
Using more than the recommended dosage of Boniva can lead to serious side effects. Do not use more Boniva than your doctor recommends.
Overdose symptoms
Symptoms of an overdose can vary depending on the form of Boniva being used. Symptoms of overdose may include:
- low blood levels of calcium, phosphate, or magnesium
- indigestion (upset stomach)
- inflammation of esophagus (the tube from your mouth to your stomach)
- swollen stomach lining
- stomach ulcer
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or your local emergency number, or go to the nearest emergency room right away.
You shouldn’t try to vomit or lie down after taking too much Boniva. Doing so can increase your risk for having an irritated esophagus. For more information, see “Serious side effects” in the “Boniva side effects” section above.
When you get Boniva tablets from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
You should store Boniva tablets at room temperature (77°F/25°C) in a tightly sealed container away from light. If needed, you may store the tablets between 59°F and 86°F (15°C and 30°C) for short periods of time, such as when traveling. Avoid storing this medication in areas where it could get damp or wet, such as bathrooms.
Disposal
If you no longer need to take Boniva and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
This article provides several useful tips on medication disposal. You can also ask your pharmacist for information on how to dispose of your medication.
The following information is provided for clinicians and other healthcare professionals.
Indications
Both Boniva tablets and Boniva injections are approved for the treatment of postmenopausal osteoporosis. Boniva tablets are also approved for the prevention of postmenopausal osteoporosis.
Administration
Boniva tablets are taken once monthly on the same day each month. Boniva tablets should be taken with 6 ounces (oz) to 8 oz of plain water. Water containing supplements, such as mineral water, should be avoided due to the higher levels of calcium.
Boniva tablets should be taken while standing or while sitting up to lessen the chance of an irritated esophagus after swallowing the drug. Patients shouldn’t lie down for at least 60 minutes after taking it. The tablets should be swallowed whole. Chewing or sucking the tablets can increase the risk of ulcers in the mouth or throat.
Boniva should be taken on an empty stomach. At least 1 hour before and 1 hour after a Boniva tablet dose, patients should avoid eating or drinking anything (other than plain water) or taking vitamins.
The Boniva injection is given by a healthcare professional once every 3 months. It’s given as an intravenous (IV) infusion over 15 to 30 seconds. An infusion is an injection into a vein that’s given over a period of time. Boniva injections should not be mixed with solutions or other intravenous drugs containing calcium.
Mechanism of action
Boniva is included under the drug classification of bisphosphonates. Boniva works by binding to hydroxyapatite (a form of calcium found in bone) to reduce the activity of osteoclasts. In turn, this slows down bone resorption and bone turnover. Generally, the bone turnover rate is higher in postmenopause. In this group of people, using Boniva also results in an overall increase in bone mass.
Pharmacokinetics and metabolism
The absorption of Boniva tablets is lessened by about 90% when taken with food or drink (except for plain water). The maximum blood concentration of Boniva occurs between 0.5 and 2 hours after oral dosing.
The half-life of Boniva is dose-dependent, ranging from 37 to 157 hours for oral Boniva and from 4.6 to 25.5 hours for injectable Boniva. Neither Boniva tablets nor the Boniva injection appear to undergo metabolism. Boniva is eliminated primarily by the kidneys, and the portion of Boniva that isn’t absorbed by the bone is excreted in the feces. A creatinine clearance less than 30 mL/min can more than double the drug exposure for both oral and injectable Boniva.
Contraindications
Boniva tablets are contraindicated in people who:
- have an irregular esophageal structure that could postpone the emptying of the esophagus after swallowing the tablet
- cannot stand or sit up for at least 1 hour after taking the drug
- have low calcium levels in their blood
- have a hypersensitivity to Boniva or any of its components
Boniva injections are contraindicated in people who:
- have low calcium blood levels
- have a hypersensitivity to Boniva or any of its components
Storage
Boniva tablets and injections should be stored at room temperature (77°F/25°C). Temporary temperature excursions are permitted between 59°F and 86°F (15°C and 30°C).
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or another healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.