Calculous cholecystitis is a gallbladder inflammation that occurs due to the presence of gallstones (cholelithiasis).
These gallstones can block the cystic duct, the channel through which bile flows from the gallbladder to the small intestine.
This blockage leads to a buildup of bile in the gallbladder, causing inflammation and infection.
This article looks at what to know about calculous cholecystitis.
Acute calculous cholecystitis is the sudden inflammation of the gallbladder due to obstruction of the cystic duct by gallstones. This condition
Chronic calculous cholecystitis is a long-term gallbladder inflammation
If a person has calculous cholecystitis, they may experience symptoms
- Severe right upper abdominal pain: The pain is sudden and intense, radiates to the right shoulder or back, and often worsens after eating fatty foods.
- Fever and chills: These indicate infection and inflammation, and general malaise often accompanies them.
- Nausea and vomiting: These are common due to irritation of the gastrointestinal tract.
- Positive Murphy’s sign: Pain and abrupt cessation of breath when someone presses the area over the gallbladder.
- Jaundice (in some cases): Yellowing of the skin and eyes can suggest the
possible involvement of the bile duct (choledocholithiasis).
Gallstones obstructing the cystic duct are the cause of acute calculous cholecystitis.
This blockage leads to a buildup of bile in the gallbladder,
Gallstones form from hardened deposits of digestive fluids,
The obstruction
Bacteria can also infect stagnant bile, leading to further inflammation and infection of the gallbladder wall.
The buildup of concentrated bile itself can also irritate and damage the gallbladder lining, contributing to inflammation.
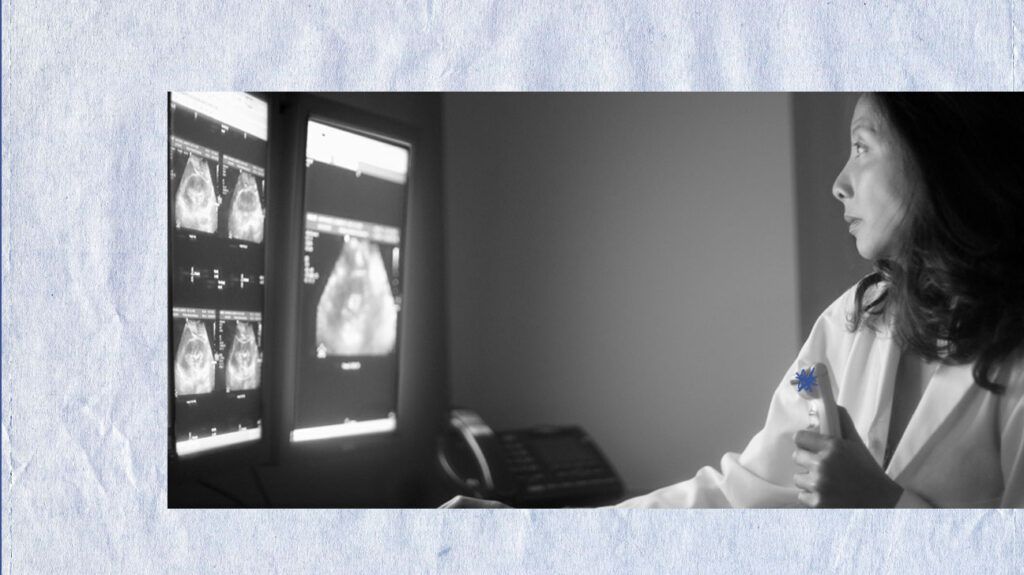
Doctors diagnose calculous cholecystitis through a combination of medical history, physical examination, and various diagnostic tests.
A doctor will ask about the nature, duration, and intensity of abdominal pain, as well as any associated symptoms such as fever, nausea, vomiting, and jaundice. They will also determine risk factors
A physical examination can check for tenderness in the right upper quadrant. Performing the Murphy’s sign test involves pressing on the upper right abdomen and asking the person to take a deep breath. Pain and a sudden halt in breath indicate a positive Murphy’s sign, suggesting gallbladder inflammation.
Blood tests a doctor may carry out include:
- Complete blood count: To check for elevated white blood cells indicating infection.
- Liver function tests:
Elevated levels of bilirubin, alkaline phosphatase, and the enzymes AST and ALT can suggest bile duct obstruction. - Pancreatic enzymes: To check amylase and lipase levels to rule out pancreatitis.
Imaging tests they may use include:
- Ultrasound: The primary and most effective imaging test for diagnosing calculous cholecystitis. It can detect gallstones, show signs of gallbladder inflammation (thickened gallbladder wall, distension), and identify fluid around the gallbladder (pericholecystic fluid).
- Hepatobiliary iminodiacetic acid (HIDA) scan: This test assesses gallbladder function and whether there is a blockage in the cystic duct if the ultrasound results are inconclusive. A nonfilling gallbladder on the HIDA scan indicates cystic duct obstruction.
- Computed tomography (CT) scan: CT scans provide detailed images of the gallbladder and surrounding structures. They help identify complications such as gallbladder perforation or abscess.
- Magnetic resonance cholangiopancreatography: This noninvasive imaging test visualizes the bile ducts and gallbladder and can detect stones in them.
The treatment of calculous cholecystitis typically
Initial medical management
- Hospitalization: Most people with acute calculous cholecystitis require admission to the hospital for close monitoring and treatment.
- Fasting (NPO): No food or drink by mouth to rest the gallbladder and reduce stimulation of bile production.
- Intravenous fluids: To maintain hydration and correct electrolyte imbalances.
- Pain management: A doctor gives analgesics to control pain.
- Antibiotics: Doctors use these to treat or prevent infection, especially if there are signs of infection (fever and elevated white blood cell count).
Cholecystectomy (gallbladder removal)
Laparoscopic cholecystectomy is the most common and preferred method. It is minimally invasive with small incisions, faster recovery, and less pain. Open cholecystectomy may be necessary in complicated cases or when laparoscopic surgery is not feasible.
Most people with calculous cholecystitis have an
The risk of severe complications exists if there is a delay to treatment or if the person has significant underlying health issues.
Removal of the gallbladder typically results in a significant reduction of symptoms and improved overall well-being.
Can acute cholecystitis go away on its own?
Acute cholecystitis typically does not resolve on its own and requires medical treatment. Without proper management, the condition
How painful is acute cholecystitis?
Acute cholecystitis is usually very painful. The pain is typically severe and localized in the upper right abdomen, often radiating to the back or right shoulder. The pain can be sharp and intense, making moving or finding a comfortable position difficult.
What is the best treatment for calculous cholecystitis?
The best treatment for calculous cholecystitis usually involves a combination of medical management and surgical intervention.
Medical management
- hospitalization and fasting to rest the gallbladder
- intravenous fluids to maintain hydration
- pain management with analgesics
- antibiotics to treat any infection
Cholecystectomy (removal of the gallbladder) is the definitive surgical treatment. Doctors can perform this laparoscopically (minimally invasive surgery) in
Understanding calculous cholecystitis is crucial for timely diagnosis and effective treatment to prevent serious complications.
If a person suspects they have symptoms of this condition, they should seek medical attention promptly.
