Xopenex is a brand-name prescription drug. It’s prescribed for people with reversible obstructive airway disease, which includes asthma and certain breathing problems related to allergies.
Xopenex is used to treat and prevent bronchospasm. This is a sudden tightening of the muscles in your airways, which causes your airways to narrow. Bronchospasm can make it hard for you to breathe.
Xopenex works quickly to help you breathe easier. Because of this, it’s called a rescue medication. Xopenex belongs to a class of medications called short-acting beta-agonists (SABAs). These drugs help the muscles in your airways to relax, which opens up your airways and makes it easier for you to breathe.
Xopenex is available in two forms, which are described below.
Xopenex vs. Xopenex HFA
Xopenex, which contains levalbuterol hydrochloride, is:
- used to treat and prevent bronchospasm in people ages 6 years and older
- a liquid solution that’s taken using a nebulizer (a machine that turns the liquid drug into a mist that can be inhaled)
Xopenex HFA, which contains levalbuterol tartrate, is:
- used to treat and prevent bronchospasm in people ages 4 years and older
- an aerosol spray that’s taken using a metered dose inhaler (an inhaler that releases puffs of the drug that can be inhaled)
Effectiveness
In clinical studies, both Xopenex and Xopenex HFA improved people’s breathing more than a placebo (treatment with no active drug) did.
In these studies, forced expiratory volume in 1 second (called FEV1) was measured to see how well people’s lungs were functioning. FEV1 is the amount of air you can force out of your lungs in 1 second. If you have certain conditions, such as asthma, your FEV1 is decreased because of tightening in your airways.
Effectiveness of Xopenex
In studies of people ages 12 years and older taking Xopenex, FEV1 was increased 35% to 40% within 30 minutes of taking the drug. In people ages 6 to 11 years, FEV1 was increased 20% to 25% after treatment. In comparison, in people from both age groups who were using a placebo, FEV1 was increased 5% to 10% after treatment.
Effectiveness of Xopenex HFA
In studies of people ages 12 years and older taking Xopenex HFA, FEV1 was increased 15% to 20% within 30 minutes of taking the drug. In comparison, people who used a placebo had their FEV1 increased by less than 5%. People ages 4 to 11 years had greater improvements in their FEV1 than did people taking a placebo. The study results seen in children were consistent with the results seen in adults.
Xopenex is available as both a brand-name and a generic medication. Xopenex contains one active ingredient: levalbuterol hydrochloride.
Xopenex HFA is also available as both a brand-name and a generic medication. Xopenex HFA contains one active drug ingredient: levalbuterol tartrate.
The Xopenex dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Xopenex to treat
- your age
- the form of Xopenex you take
- other medical conditions you may have
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug forms and strengths
Xopenex comes in these two forms:
- a liquid solution, called Xopenex
- an aerosol spray, called Xopenex HFA
The strengths and dosages for each of these forms are described below.
Xopenex
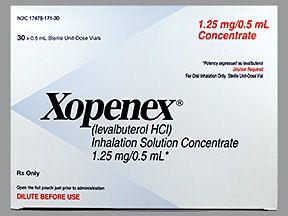
Xopenex (levalbuterol hydrochloride) comes as a liquid solution that’s taken using a nebulizer. With a nebulizer, the liquid solution is turned into a mist, which can be inhaled. This form of Xopenex comes in single-dose vials. It’s available in the following strengths:
- 0.31 mg/3 mL
- 0.63 mg/3 mL
- 1.25 mg/3 mL
Xopenex is also available in a concentrated liquid solution that comes in one strength: 1.25 mg/0.5 mL. This solution has to be diluted before it can be taken with your nebulizer.
Xopenex HFA
Xopenex HFA (levalbuterol tartrate) comes as an aerosol spray that’s taken using a metered dose inhaler (MDI). With an MDI, the drug is released in a puff, which can be inhaled. Each actuation (release of the puff) from the inhaler gives 59 mcg of Xopenex HFA, which equals 45 mcg of levalbuterol.
Xopenex HFA comes in 15-gram aerosol canisters (which each hold 200 actuations). The canisters will each last for a different number of doses, depending on how often you use them and how many puffs you take for each dose.
Dosage for bronchospasm
Xopenex is used as a rescue medication. This means it’s used as needed to treat sudden breathing problems. The typical dosage of Xopenex and Xopenex HFA varies from person to person.
Dosage of Xopenex for bronchospasm
For people ages 12 years and older, the typical dosage of Xopenex is 0.63 mg, taken up to three times daily (every 6 to 8 hours) with a nebulizer. The typical dosage for children ages 6 through 11 years is described below, in the section “Pediatric dosing.”
Your doctor may prescribe a dosage for you that’s higher than the typical dosage. The maximum dosage of Xopenex is usually 1.25 mg taken three times daily.
Dosage of Xopenex HFA for bronchospasm
For people ages 4 years and older, the typical dosage of Xopenex HFA is two puffs (a total of 90 mcg) taken up to every 4 to 6 hours. Higher or more frequent doses of Xopenex HFA aren’t typically prescribed.
If your breathing condition is mild, your doctor may only prescribe one puff (45 mcg) of Xopenex HFA taken up to every 4 hours.
Pediatric dosage
For Xopenex, the typical dosage in children ages 6 through 11 years is 0.31 mg taken up to three times each day by nebulization.
The maximum dosage of Xopenex in this age group is usually 0.63 mg taken up to three times daily. This also happens to be the starting dosage of Xopenex for adults and children ages 12 and older.
For Xopenex HFA, the dosage for children is the same as it is for adults. See the section “Dosage of Xopenex HFA for bronchospasm” above for details.
What if I miss a dose?
Unless your doctor tells you otherwise, you’ll only take Xopenex as needed for sudden breathing problems. You won’t need to take it regularly when you’re not having symptoms. This is because Xopenex is considered a rescue medication. It begins working quickly after it’s taken to help improve your breathing symptoms right away.
If you need to take Xopenex more than twice each week to treat your breathing problems, your doctor may change your overall treatment plan.
Will I need to use this drug long term?
Possibly. Xopenex is meant to be used “as needed” to treat sudden breathing problems. If this medication is working well for you, your doctor may recommend that you continue to use it over a long period of time.
You may wonder how Xopenex compares to other medications that are prescribed for similar uses. Here we look at how Xopenex, Xopenex HFA, and albuterol are alike and different.
About
Xopenex contains the drug levalbuterol hydrochloride, while Xopenex HFA contains the drug levalbuterol tartrate. Albuterol is a drug that’s available as both generic and brand-name medications.
All three of these drugs belong to a class of medications called short-acting beta-agonists (SABAs). They’re also called rescue medications because they work quickly to treat sudden breathing problems.
Uses
Xopenex, Xopenex HFA, and albuterol are each used as needed to treat and prevent bronchospasm in people with reversible obstructive airway disease. With bronchospasm, the main airways in your lungs become tight and narrow. This can make it hard for you to breathe. Reversible obstructive airway disease includes conditions such as asthma and certain other breathing problems related to allergies.
Xopenex is prescribed for people ages 6 years and older, while Xopenex HFA is prescribed for people ages 4 years and older.
Depending on the form of albuterol prescribed, it can sometimes be used in people as young as 2 years of age. However, some forms of albuterol can’t be used in people younger than 6 years of age.
Albuterol can also be used to prevent exercise-induced bronchospasm in people ages 4 years and older. With this condition, you have trouble breathing during exercise.
Drug forms and administration
Xopenex comes as a liquid solution that’s taken using a nebulizer. With a nebulizer, the liquid solution is turned into a mist, which can be inhaled.
Xopenex HFA comes as an aerosol spray that’s taken using a metered dose inhaler (MDI). With an MDI, the drug is released in puffs, which can be inhaled.
Albuterol comes in several different forms. Examples of these forms include:
- aerosol spray, which is taken using an MDI:
- albuterol (ProAir HFA, Proventil HFA, Ventolin HFA)
- powder, which is taken with a dry-power inhaler:
- albuterol (ProAir RespiClick)
- liquid solution, which is taken using a nebulizer:
- albuterol sulfate (AccuNeb)
- oral syrup or tablet, which are each taken by mouth (swallowed):
- albuterol sulfate (VoSpire ER)
Side effects and risks
Xopenex, Xopenex HFA, and albuterol are very similar drugs, which means they can cause similar side effects. Below are examples of these side effects.
More common side effects
The more common side effects that can occur with Xopenex, Xopenex HFA, or albuterol (when they’re taken individually) include:
- bronchitis (inflammation in your airways), which can cause cough or wheezing
- diarrhea
- vomiting
- headache
- fast heart rate
- dizziness
- sore throat
- runny or stuffy nose
- general pain in your body
- pain in your ears or chest
- being more prone to accidents, which may lead to physical injury
- nervousness
- tremor
- infections, such as certain viral infections or urinary tract infections (UTIs)
- palpitations (feeling fluttering with your heartbeat)
Serious side effects
The serious side effects that can occur with Xopenex, Xopenex HFA, or albuterol (when they’re taken individually) include:
- severe bronchospasm (tightening of your airways) that can be life-threatening
- heart problems, including very fast heart rate, severe palpitations, or changes in your blood pressure
- severe allergic reaction
- low potassium level
Effectiveness
Xopenex, Xopenex HFA, and albuterol are all approved to treat and prevent bronchospasm in people with reversible obstructive airway disease.
Effectiveness of Xopenex HFA vs. albuterol HFA
Both Xopenex HFA and albuterol HFA have been shown effective in treating bronchospasm related to asthma.
The use of Xopenex HFA and albuterol HFA to treat bronchospasm related to asthma was directly compared in clinical studies. In the studies, people’s forced expiratory volume in 1 second (FEV1) was measured to see how well their lungs were functioning. Higher FEV1s indicate better lung function than lower FEV1s.
After 8 weeks of treatment, people taking either albuterol HFA or Xopenex HFA had their peak FEV1 increase by 15% to 20%. In people taking a placebo (treatment with no active drug), their peak FEV1 was increased by 5%.
Effectiveness of nebulized Xopenex vs. nebulized albuterol
The use of nebulized Xopenex and nebulized albuterol have also been directly compared in clinical studies of people with mild to moderate asthma. In the studies, people’s FEV1 (forced expiratory volume in 1 second) was measured to see how well their lungs were functioning. Larger FEV1s indicate better lung function than smaller FEV1s.
In this 4-week study, some people were given either Xopenex or albuterol sulfate three times daily. Other people were given a placebo (treatment with no active drug).
In adults taking Xopenex, peak FEV1 was increased by 40% to 45% on their first day of treatment. Of adults taking albuterol, peak FEV1 increased by 35% on their first day of treatment.
In children ages 6 to 11 years, peak FEV1 was increased by 23% to 27% on the first day of treatment for those taking Xopenex. Children in this age group who were taking 2.5 mg of albuterol had about the same increase in their FEV1. However, children taking 1.25 mg of albuterol had their peak FEV1 increase by 15% to 20% on the first day of treatment.
All the people in the study who were using either Xopenex or albuterol had their FEV1 increase more than did people who were taking a placebo.
Costs
Xopenex and Xopenex HFA are each available as brand-name and generic medications. Albuterol is available in several forms, which come in both brand-name and generic options.
The generic version of Xopenex, Xopenex HFA, and certain forms of albuterol generally cost about the same. Brand-name Xopenex and Xopenex HFA are much more expensive than the generic form of either drug. Brand-name medications usually cost more than generics.
The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Xopenex and Xopenex HFA can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Xopenex or Xopenex HFA. These lists do not include all possible side effects.
For more information on the possible side effects of Xopenex or Xopenex HFA, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Xopenex, you can do so through MedWatch.
More common side effects
The more common side effects of Xopenex and Xopenex HFA can include:
- bronchitis (inflammation in your airways), which can cause cough or wheezing
- diarrhea
- vomiting
- headache
- fast heart rate
- dizziness
- sore throat
- runny or stuffy nose
- general body pain
- pain in your ears or chest
- being more prone to accidents, which may lead to physical injury
- nervousness
- tremor
- infections, such as viral infections or urinary tract infections (UTIs)
- palpitations (feeling fluttering with your heartbeat)
Many of these side effects may go away or become less noticeable over time. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Xopenex and Xopenex HFA aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
One serious side effect of Xopenex and Xopenex HFA is severe bronchospasm (tightening of your airways). Symptoms of this condition can include:
- shortness of breath
- wheezing
- tightness in your chest
- cough
Other serious side effects, which are discussed more in the section “Side effect details” below, include:
- severe allergic reaction
- heart-related problems, such as very fast heart rate, severe palpitations, and changes in your blood pressure
- paradoxical bronchospasm (tightening of your airways that’s unexpected since the drug is meant to treat bronchospasm)
- low potassium level
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on several of the side effects this drug may cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Xopenex or Xopenex HFA. In clinical studies, no one taking Xopenex had an allergic reaction to the drug. It’s not known for sure if anyone had an allergic reaction to Xopenex HFA.
Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Xopenex. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
Tachycardia or other heart problems
You may feel your heart rate increase (called tachycardia) after taking a dose of Xopenex or Xopenex HFA. This side effect will likely go away after several hours following your dose.
In clinical studies of people ages 12 years and older using Xopenex, about 3% of people had tachycardia. No one taking a placebo (treatment with no active drug) had tachycardia.
Other heart-related side effects that may be caused by Xopenex and Xopenex HFA include:
- changes in your blood pressure
- palpitations (feeling fluttering with your heartbeat)
It’s not known for sure how often these other heart-related side effects occurred in people during clinical studies.
If you have any heart problems while you’re taking Xopenex or Xopenex HFA, tell your doctor right away. If you have chest pain or palpitations, or your heart is racing, call your doctor immediately. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
If you have heart-related side effects from Xopenex or Xopenex HFA, your doctor may recommend that you use a different medication for your breathing problems.
Upper respiratory infections
You may have upper respiratory infections, such as the common cold, while you’re using Xopenex or Xopenex HFA. These infections can cause cough, runny or stuffy nose, and sore throat.
In clinical studies of people ages 12 years and older, viral respiratory infections occurred in 7% to 12% of people taking Xopenex. Of those taking a placebo (treatment with no active drug), 9% had the same result.
In other clinical studies, sore throat or a runny or stuffy nose was reported in 7% to 8% of people ages 12 and older taking Xopenex HFA. Of people taking a placebo, 2% to 3% had the same result.
If you develop an upper respiratory infection while you’re using Xopenex or Xopenex HFA, your symptoms should go away after about a week. However, if they don’t go away, or if your breathing problems worsen, talk with your doctor. They can check to see if you have an infection and recommend whether you need any additional treatment.
Paradoxical bronchospasm
Some people have paradoxical (unexpected) bronchospasm when using Xopenex or Xopenex HFA. With bronchospasm, your airways become tight and narrow, making it hard for you to breathe. This side effect isn’t expected since these drugs are meant to treat and prevent bronchospasm.
Symptoms of bronchospasm can include:
- shortness of breath
- wheezing
- tightness in your chest
- cough
Paradoxical bronchospasm typically happens right after you’ve taken a dose of Xopenex or Xopenex HFA. It’s also more likely to happen when you’re using a new canister or vial of the drug for the first time.
If you have unexpected bronchospasm after taking Xopenex or Xopenex HFA, stop taking the drug and call your doctor right away. Call 911 if your symptoms feel life-threatening or if you think you’re having a medical emergency.
If you have worsened breathing problems while using Xopenex or Xopenex HFA, your doctor may prescribe a different medication for you.
Low potassium level
Xopenex and Xopenex HFA can cause a low potassium level (hypokalemia) in people using these drugs. This side effect is usually temporary and typically doesn’t require medical treatment. Symptoms of hypokalemia can include:
- fainting
- tingling or numbness
- muscle cramps
- abnormal heart rate
- irregular heartbeat pattern
If you’re having symptoms of low potassium, your doctor may order a blood test to check your potassium level. A low potassium level can be dangerous to your health, especially if it doesn’t go away.
Talk with your doctor if you’re having symptoms of a low potassium level during treatment. Your doctor will make sure that your level is safe while you’re using Xopenex or Xopenex HFA.
Side effects in children
During clinical studies of Xopenex and Xopenex HFA, the side effects in children were very similar to those in adults.
The Food and Drug Administration (FDA) approves prescription drugs such as Xopenex and Xopenex HFA to treat certain conditions. Xopenex and Xopenex HFA may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Xopenex for bronchospasm
Xopenex and Xopenex HFA are FDA-approved to treat and prevent bronchospasm in people with reversible obstructive airway disease. With bronchospasm, the main airways in your lungs become tight and narrow, making it hard for you to breathe.
Reversible obstructive airway disease includes conditions such as asthma and other certain breathing problems related to allergies. Symptoms of these conditions may fluctuate during your lifetime, but it’s likely that you’ll need to treat your condition long term. Typical symptoms of reversible obstructive airway disease include cough, chest tightness, and trouble breathing.
Xopenex is approved for use in people ages 6 years and older, while Xopenex HFA is approved for use in people ages 4 years and older.
These drugs belong to a class of medications called short-acting beta-agonists (SABAs). They’re also known as rescue medications because they work quickly to relax the muscles in your airways. This opens up your airways and makes it easier for you to breathe.
Effectiveness for bronchospasm
In clinical studies, both Xopenex and Xopenex HFA improved people’s breathing more than a placebo (treatment with no active drug) improved their breathing.
In these studies, forced expiratory volume in 1 second (called FEV1) was measured to see how well people’s lungs were functioning. FEV1 is the amount of air you can force out of your lungs in 1 second. If you have certain conditions, such as asthma, your FEV1 is decreased because of tightening in your airways.
Effectiveness of Xopenex for bronchospasm
In studies of people ages 12 years and older taking Xopenex, FEV1 was increased 35% to 40% within 30 minutes of taking the drug. In people ages 6 to 11 years, FEV1 was increased 20% to 25% after treatment. In comparison, in people from both age groups who were using a placebo, FEV1 was increased 5% to 10% after treatment.
Effectiveness of Xopenex HFA for bronchospasm
In studies of people ages 12 years and older taking Xopenex HFA, FEV1 was increased 15% to 20% within 30 minutes of taking the drug. In comparison, people using a placebo (treatment with no active drug) had their FEV1 increased by less than 5%.
People ages 4 to 11 years had greater improvements in their FEV1 than did people taking a placebo. The study results seen in children were consistent with the results seen in adults.
Off-label uses for Xopenex
In addition to the use listed above, Xopenex and Xopenex HFA may be used off-label. Off-label drug use is when a drug that’s approved for one use is used for a different one that’s not approved.
Xopenex for COPD (off-label use)
Xopenex and Xopenex HFA aren’t approved to treat chronic obstructive pulmonary disease (COPD), but sometimes they’re used off-label for this condition. COPD includes conditions such as chronic bronchitis and emphysema.
There isn’t a cure for COPD, but COPD symptoms can be treated. Xopenex and Xopenex HFA can help treat sudden COPD symptoms (called flare-ups). Since these drugs aren’t approved for this use, typical dosages for people with COPD haven’t been recommended in treatment guidelines. Your doctor will work with you to create a treatment plan that works best to manage your COPD symptoms.
If you’d like to know more about using Xopenex or Xopenex HFA to treat COPD, talk with your doctor.
Xopenex for exercise-induced bronchospasm prevention (off-label use)
Xopenex HFA isn’t approved to prevent exercise-induced bronchospasm, but sometimes it’s used off-label for this condition in adults and children.
With exercise-induced bronchospasm, you may have shortness of breath and chest tightness when you’re exercising. Using a medication such as Xopenex HFA about 15 minutes before you start exercising can help prevent these symptoms.
A
If you have questions about using Xopenex or Xopenex HFA for exercise-induced bronchospasm, talk with your doctor. They can discuss all of your treatment options with you.
Xopenex and children
Xopenex is approved for use in children ages 6 years and older, while Xopenex HFA is approved for use in children ages 4 years and older. For more information on the conditions these drugs are used to treat, see the section “Xopenex for bronchospasm” above.
Xopenex and Xopenex HFA are short-acting medications that are used as needed to treat sudden breathing problems. These drugs are also called rescue inhalers or rescue medications. They work quickly to treat breathing problems, such as shortness of breath and chest tightness.
Rescue medications are almost always used with drugs called maintenance medications. When used to treat breathing problems such as asthma, maintenance medications are taken consistently, at least once every day. Maintenance medications are used to prevent breathing conditions from worsening and to prevent sudden breathing symptoms.
Examples of maintenance medications used to treat certain breathing conditions include:
- certain inhaled corticosteroids, such as:
- beclomethasone (Qvar)
- budesonide (Pulmicort)
- ciclesonide (Alvesco)
- flunisolide (Aerospan)
- fluticasone (Flovent)
- mometasone (Asmanex)
- certain long-acting beta-agonists, such as:
- salmeterol (Serevent)
- formoterol (Perforomist)
- certain drugs that contain a combination of an inhaled corticosteroid and a long-acting beta-agonists, such as:
- fluticasone/salmeterol (Advair)
- budesonide/formoterol (Symbicort)
- mometasone/formoterol (Dulera)
- certain leukotriene receptor antagonists, such as:
- montelukast (Singulair)
- zafirlukast (Accolate)
- certain oral corticosteroids, such as:
- methylprednisolone (Medrol)
- prednisolone (Orapred ODT)
- prednisone (Rayos)
- certain immunomodulators, such as:
- omalizumab (Xolair)
If you need to use your rescue medication, such as Xopenex or Xopenex HFA, more than twice each week, let your doctor know. They may recommend changing your maintenance medication to something that better controls your breathing symptoms. This way, you won’t need to use your rescue medication as often.
Other drugs are available that can treat or prevent bronchospasm caused by reversible obstructive airway disease. Some drugs may be better suited for you than others. If you’re interested in finding an alternative to Xopenex, talk with your doctor. They can tell you about other medications that may work well for you.
Xopenex and Xopenex HFA belong to a class of drugs called short-acting beta-agonists (SABAs). These drugs work quickly to treat sudden breathing problems, such as shortness of breath or chest tightness. Drugs that work in this way are called rescue medications.
Examples of other medications that can be used to treat bronchospasm include:
- other SABAs, such as albuterol (Ventolin, ProAir, AccuNeb)
- medications that contain a combination of a SABA and an anticholinergic drug, such as ipratropium bromide/albuterol sulfate (Combivent Respimat, DuoNeb)
Note: Some of the drugs listed above are used off-label to treat this condition. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
You may wonder how Xopenex compares to other medications that are prescribed for similar uses. Here we look at how Xopenex, Xopenex HFA, and Pulmicort are alike and different.
About
Xopenex contains the drug levalbuterol hydrochloride, while Xopenex HFA contains the drug levalbuterol tartrate. These drugs belong to a class of medications called short-acting beta-agonists (SABAs).
Pulmicort contains the drug budesonide. It belongs to a class of medications called inhaled corticosteroids.
Uses
Xopenex and Xopenex HFA are used as needed to treat and prevent bronchospasm in people with reversible obstructive airway disease. With bronchospasm, the main airways in your lungs become tight and narrow, making it hard for you to breathe. Reversible obstructive airway disease includes conditions such as asthma and certain other breathing problems related to allergies.
Xopenex can be prescribed for people ages 6 years and older, while Xopenex HFA can be prescribed for people ages 4 years and older. These drugs are called rescue medications because they work quickly to treat sudden breathing problems.
Pulmicort, on the other hand, is used as a maintenance treatment for asthma. As a maintenance treatment, this drug is taken consistently rather than as needed. It works to control asthma symptoms and prevent sudden breathing problems (called flare-ups). Pulmicort is not a rescue inhaler, and it shouldn’t be used to treat bronchospasm or other sudden breathing problems.
Pulmicort Flexhaler (an aerosol powder) can be given to people ages 6 years and older. Pulmicort Respules (a liquid suspension) can be given to people ages 12 months to 8 years of age.
Drug forms and administration
Xopenex comes as a liquid solution that’s taken as needed using a nebulizer. With a nebulizer, the liquid solution is turned into a mist, which can be inhaled.
Xopenex HFA comes as an aerosol spray that’s taken as needed using a metered dose inhaler (MDI). With an MDI, the drug is released in puffs, which can be inhaled.
Pulmicort comes as an aerosol powder (called Pulmicort Flexhaler) that’s taken using a dry powder inhaler. Pulmicort Flexhaler is typically taken once or twice each day. Pulmicort also comes as a liquid suspension (called Pulmicort Respules) that’s taken using a nebulizer. This form of Pulmicort is typically taken twice each day.
Side effects and risks
Xopenex and Xopenex HFA belong to a different class of medications than Pulmicort. Therefore, these drugs can cause similar and different side effects. Below are examples of both common and serious side effects for each drug.
More common side effects
These lists contain examples of more common side effects that can occur with Xopenex, Xopenex HFA, Pulmicort, or each of the drugs (when they’re taken individually).
- Can occur with Xopenex:
- fast heart rate
- dizziness
- general body pain
- pain in your ears or chest
- being more prone to accidents, which may lead to physical injury
- nervousness
- tremor
- palpitations (feeling fluttering with your heartbeat)
- Can occur with Pulmicort:
- fungal infections, such as Candida albicans infection, in your mouth and throat
- otitis media (middle ear infection)
- nose bleeds
- decreased appetite
- Can occur with both Xopenex and Pulmicort:
- respiratory infections, which may cause cough and runny or stuffy nose
- infections, which may include viral infections, upper respiratory infections, urinary tract infections (UTIs), or eye infections
- digestive system problems, such as vomiting, diarrhea, or belly pain
- bronchitis (inflammation in your airways), which may cause cough or wheezing
- headache
- sore throat
Serious side effects
These lists contain examples of serious side effects that can occur with Xopenex, Xopenex HFA, Pulmicort, or each of the drugs (when they’re taken individually).
- Can occur with Xopenex:
- heart problems, such as very fast heart rate, severe palpitations, and changes in your blood pressure
- low potassium level
- Can occur with Pulmicort
- decreased ability of your immune system to protect against infections
- increased levels of a hormone called cortisol, which may suppress the activity of your adrenal glands
- reduced bone density
- slowed growth in children using the drug
- eye problems, such as glaucoma (increased pressure in your eye) and cataracts (cloudiness in the lens of your eye)
- Can occur with both Xopenex and Pulmicort
- severe bronchospasm (tightening of your airways)
- severe allergic reaction
Effectiveness
Xopenex and Pulmicort have different approved uses, but they’re both used to treat asthma or other forms of reversible obstructive airway disease.
These drugs haven’t been directly compared in clinical studies. But separate studies have found both Xopenex and Xopenex HFA to be effective as a rescue (as needed) treatment of bronchospasm that’s related to reversible obstructive airway disease.
Studies have also found Pulmicort Flexhaler and Pulmicort Respules to be effective as maintenance (consistent) treatment of asthma to control breathing problems and prevent flare-ups. However, Pulmicort isn’t approved and shouldn’t be used as a rescue treatment for bronchospasm.
Costs
Xopenex and Pulmicort are available as both generic and brand-name drugs. Brand-name medications usually cost more than generics.
Generic forms of Xopenex are generally less expensive than generic forms of Pulmicort. The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Here are answers to some frequently asked questions about Xopenex and Xopenex HFA.
Can I use Xopenex with Atrovent?
Yes, Xopenex and Xopenex HFA are each sometimes prescribed for use with Atrovent (ipratropium).
Xopenex and Xopenex HFA are short-acting medications that are used as needed to treat sudden breathing symptoms. They’re also called rescue medications. Xopenex shouldn’t be used routinely every day. It’s meant to be used only as needed.
On the other hand, Atrovent is a maintenance medication. It’s meant to be used consistently to control breathing problems and prevent sudden flare-ups. But even with maintenance treatment, some people still need to use a rescue medication occasionally. In these cases, Xopenex or Xopenex HFA may be prescribed to be used with Atrovent.
Atrovent is available by itself and also as part of a combination medication that contains albuterol. (Albuterol is a short-acting medication that’s very similar to Xopenex.) This combination product is typically used as a rescue medication.
If you’re taking this combination medication, talk with your doctor before starting Xopenex. Your doctor may recommend a different treatment plan for you so that you avoid taking two rescue medications.
Is Xopenex a corticosteroid?
No, Xopenex and Xopenex HFA aren’t corticosteroids. They’re called short-acting beta-agonists (SABAs). Xopenex and Xopenex HFA are used as needed to treat sudden breathing problems. They work quickly to open your airways and make it easier for you to breathe. Because of this, they’re also called rescue medications.
Corticosteroids are commonly used as maintenance medications to control asthma or other breathing conditions and prevent flare-ups. Maintenance medications are taken consistently each day, rather than as needed.
Corticosteroids are available as inhaled and oral (taken by mouth) forms. Sometimes, corticosteroids are used with rescue medications as part of your complete treatment plan. For more information on this, see the section “Xopenex use with other drugs” above.
Some examples of corticosteroids that are used to treat breathing conditions include:
- budesonide (Pulmicort)
- fluticasone (Flovent)
- mometasone (Asmanex)
If you have questions about whether you need to use corticosteroids, talk with your doctor about your treatment options.
Will I need to use other COPD or asthma drugs with Xopenex?
Yes, you’ll likely need to use other drugs while you’re taking Xopenex or Xopenex HFA.
Xopenex and Xopenex HFA are short-acting medications that are used as needed to treat sudden breathing symptoms. These drugs work quickly to help you breathe easier. Because of this, they’re called rescue medications.
Other drugs, called maintenance medications, are used consistently (at least once each day). These drugs work to control breathing conditions and prevent symptom flare-ups. If maintenance drugs are working well for you, you shouldn’t need to use your rescue medication very often.
Xopenex and Xopenex HFA should generally be used less than twice each week. If you need to use them more often, talk with your doctor. They may recommend adjusting your maintenance medication so that you don’t need to use your rescue medication as often.
If you have questions about which medications you’ll need to take with Xopenex, talk with your doctor.
Is there a maximum number of times that I can use Xopenex each day or each week?
In general, treatment guidelines for rescue medications, such as Xopenex or Xopenex HFA, recommend that you shouldn’t need to use the drugs more than twice weekly. Rescue medications are used as needed to treat sudden breathing problems. They aren’t meant to be taken consistently each day.
If you do need to use your rescue medication more than twice a week, your doctor may recommend adjusting your treatment plan. This could include making changes to any other drugs you’re using with Xopenex or Xopenex HFA.
Listed below are the maximum recommended dosages for Xopenex and Xopenex HFA, when these drugs are used to treat bronchospasm related to asthma. If you have questions about how often you should be using Xopenex or Xopenex HFA, talk with your doctor.
Xopenex maximum daily dosage when used in people with asthma
In people ages 12 years and older, the maximum dosage of Xopenex is usually 1.25 mg taken three times daily. For people ages 6 through 11 years, the maximum dosage is usually 0.63 mg taken three times daily.
Xopenex HFA maximum daily dose when used in people with asthma
In people ages 4 years and older, the maximum dosage of Xopenex HFA is usually two puffs (a total of 90 mcg) taken once every 4 hours.
There aren’t any known interactions between alcohol and Xopenex or between alcohol and Xopenex HFA.
Talk with your doctor about whether it’s safe for you to consume alcohol while you’re taking either of these drugs. If you have certain heart problems (such as blood pressure issues or heart palpitations) or you drink large amounts of alcohol, you may be more likely to have side effects from these medications.
Your doctor can recommend whether it’s safe for you to drink alcohol while you’re using Xopenex or Xopenex HFA.
Xopenex can interact with several other medications. It can also interact with certain supplements.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Xopenex and other medications
Below are lists of medications that can interact with Xopenex. These lists do not contain all the drugs that may interact with Xopenex.
Before taking Xopenex, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Xopenex and albuterol
Using either Xopenex or Xopenex HFA with albuterol can increase your risk of serious side effects. This includes heart-related side effects such as chest pain, palpitations (feeling fluttering with your heartbeat), or changes in your blood pressure.
You shouldn’t take albuterol with Xopenex or Xopenex HFA.
Xopenex and certain heart medications
Using either Xopenex or Xopenex HFA with certain heart medications can cause drug interactions. Examples of heart medications that may interact with Xopenex or Xopenex HFA include:
- diuretics, such as:
- hydrochlorothiazide (Microzide)
- furosemide (Lasix)
- bumetanide (Bumex)
- beta-blockers, such as:
- atenolol (Tenormin)
- metoprolol (Toprol)
- bisoprolol (Zebeta)
- labetalol (Trandate)
- digoxin (Lanoxin)
Interactions with these drugs are described below. Talk with your doctor before taking diuretics, beta-blockers, or digoxin while you’re using Xopenex.
Xopenex and diuretics
Taking diuretics, Xopenex, or Xopenex HFA can lower your potassium level. Taking these medications together can further increase your risk of having a low potassium level. Symptoms of low potassium level include muscle cramps, problems with your heart rhythm, dizziness, and fainting.
Typically, changes in your potassium level that are caused by taking Xopenex or Xopenex HFA are temporary. And your potassium level usually returns to normal without being treated. But this may not be the case if you’re taking a diuretic with either Xopenex or Xopenex HFA.
If you need to take a diuretic, your doctor will likely recommend that you use a drug other than Xopenex or Xopenex HFA.
Xopenex and beta-blockers
Taking beta-blockers with either Xopenex or Xopenex HFA can lower the effectiveness of Xopenex or Xopenex HFA to treat your breathing problems. Using beta-blockers with either of these drugs can also make you more prone to having bronchospasm (tightening of your airways that can make it hard for you to breathe).
If you need to take a beta-blocker, your doctor will likely recommend that you use a drug other than Xopenex or Xopenex HFA.
Xopenex and digoxin
Using either Xopenex or Xopenex HFA with digoxin may decrease the level of digoxin (Lanoxin) in your body. This can make digoxin less effective to treat your condition.
If you’re taking digoxin, your doctor will probably check your digoxin level soon after you start using either Xopenex or Xopenex HFA. Your doctor may monitor your digoxin level more often than usual if you’re taking digoxin with either of these drugs.
In some cases, your doctor may recommend that you use a drug other than Xopenex or Xopenex HFA if you need to take digoxin.
Xopenex and certain antidepressants
Using either Xopenex or Xopenex HFA with certain antidepressants can cause drug interactions. Examples of these antidepressant medications include:
- monoamine oxidase inhibitors (MAOIs), such as:
- selegiline (Emsam)
- phenelzine (Nardil)
- tricyclic antidepressants, such as:
- amitriptyline
- desipramine (Norpramin)
- nortriptyline (Pamelor)
If you’ve taken any of these antidepressants within 2 weeks of using either Xopenex or Xopenex HFA, you may be more likely to have heart-related side effects. These side effects can include fast heart rate, palpitations (feeling fluttering with your heartbeat), or changes in your blood pressure.
These antidepressant medications shouldn’t be taken at the same time as or within 2 weeks of using either Xopenex or Xopenex HFA.
If you need to take an MAOI or a tricyclic antidepressant, your doctor will likely recommend that you use a drug other than Xopenex or Xopenex HFA.
Xopenex and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Xopenex. However, you should still check with your doctor or pharmacist before using any of these products while taking Xopenex.
Using more than the recommended dosage of Xopenex or Xopenex HFA can lead to serious side effects. Sometimes severe, life-threatening side effects can occur with overuse or misuse of these drugs.
Overdose symptoms
Symptoms of an overdose can include:
- seizures
- chest pain
- very fast heart rate (sometimes up to 200 beats each minute)
- palpitations (feeling fluttering with your heartbeat)
- dizziness
- nervousness
- anxiety
- cardiac arrest (when your heart stops beating)
- in serious cases, death
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
It’s not known for sure if Xopenex and Xopenex HFA are safe for use during pregnancy. Studies are currently being done to better understand if these drugs have an effect on pregnant women or on their developing fetuses. If you’d like to know more about these studies or want to register to participate in them, visit the program website.
Animal studies have looked at using Xopenex and Xopenex HFA in pregnant females. The doses of these drugs given in the studies were higher than typical doses given to humans. No negative effects were seen in fetuses exposed to either drug. But keep in mind that animal studies don’t always predict what will happen in humans. More studies are needed to know if these drugs affect human pregnancies.
It’s also important to know that unmanaged or poorly managed asthma can have negative effects on a mother and unborn baby during pregnancy. If you’re pregnant and you have reversible obstructive airway disease, such as asthma, talk with your doctor. They can discuss with you the risks and benefits of different treatment options.
It’s not known if Xopenex is safe to take during pregnancy. If you or your sexual partner can become pregnant, talk with your doctor about your birth control needs while you’re using Xopenex.
It’s not known if Xopenex and Xopenex HFA pass into human breast milk. It’s also not known how these medications may affect a child who’s breastfed.
Talk with your doctor if you’re breastfeeding, or considering breastfeeding, while you’re taking Xopenex or Xopenex HFA. Your doctor can recommend healthy and safe ways to feed your child.
As with all medications, the cost of Xopenex and Xopenex HFA can vary.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your insurance plan may require you to get prior authorization before they approve coverage for Xopenex. This means that your doctor will need to send a request to your insurance company asking them to cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Xopenex.
If you’re not sure if you’ll need to get prior authorization for Xopenex, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Xopenex HFA, or if you need help understanding your insurance coverage, help is available.
Sunovion Pharmaceuticals Inc., the manufacturer of Xopenex HFA, has reimbursement specialists who can give you information about the cost of Xopenex HFA. For more information, call 844-276-8262.
If you’d like to know about ways to save on Xopenex, talk with your doctor or pharmacist.
You should take Xopenex according to your doctor or healthcare provider’s instructions.
When and how to take
Xopenex and Xopenex HFA are each used as needed to treat and prevent bronchospasm caused by certain breathing conditions. With bronchospasm, your airways becomes tight and narrow, which makes it hard for you to breathe.
Information on how to take both Xopenex and Xopenex HFA is described below.
How to take Xopenex
Xopenex comes as a liquid solution that’s taken using a nebulizer. With a nebulizer, the liquid medication is turned into a mist that you’ll inhale.
After you’ve put Xopenex solution inside of your nebulizer, you’ll place the nebulizer mask over your nose and mouth. You’ll inhale the misted medication as you breathe through the mask. It generally takes about 5 to 15 minutes for each treatment.
Instructions for how to use your nebulizer will be specific to your machine. Read the manufacturer’s instructions for your machine to be sure you know how to operate the nebulizer.
Children or older adults who are taking Xopenex may need help to set up and use their nebulizer. This helps to make sure that they’re getting the correct dose of Xopenex.
How to take Xopenex HFA
Xopenex HFA comes as an aerosol spray that’s taken using a metered dose inhaler (MDI). With an MDI, the drug is released in puffs, which are inhaled.
You’ll need to take deep, slow breaths with the MDI to make sure that you inhale all of the medication into your lungs. For some people, using an MDI is more difficult than using a nebulizer.
For additional instructions on how to use Xopenex HFA, see the manufacturer’s website.
What if I miss a dose?
Unless your doctor tells you otherwise, you’ll take Xopenex or Xopenex HFA only as needed when you’re having sudden breathing problems. You won’t need to take these drugs consistently on a schedule, unless your doctor recommends that you do so.
Xopenex and Xopenex HFA are short-acting beta-agonists (beta agonists). They work to treat bronchospasm that’s associated with reversible obstructive airway disease. Examples of reversible obstructive airway disease include conditions such as asthma and certain other breathing problems that are related to allergies.
With bronchospasm, the main airways in your lungs become tight and narrow, making it hard for you to breathe. Xopenex and Xopenex HFA work by quickly relaxing the muscles in your airways, which makes it easier for you to breathe.
How long does it take to work?
After taking each dose of Xopenex or Xopenex HFA, your breathing symptoms should be noticeably improved within about 15 minutes. These medications will continue to work for several hours after they’re taken.
Xopenex and Xopenex HFA are considered rescue medications because they work quickly to treat symptoms when they occur.
Before taking Xopenex or Xopenex HFA, talk with your doctor about your health history. Xopenex may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Certain heart conditions. Xopenex and Xopenex HFA may cause heart-related side effects, such as fast heart rate, palpitations, or changes in your blood pressure. If you have certain heart conditions, you may have an increased risk of these side effects. If you have any heart or blood pressure problems, talk with your doctor before you start taking Xopenex or Xopenex HFA.
- Allergy to levalbuterol or albuterol. You should not take Xopenex or Xopenex HFA if you’ve had an allergic reaction in the past to either albuterol or levalbuterol (the active drug in Xopenex and Xopenex HFA). Talk with your doctor about any history of drug allergies before starting any new medications.
- Low potassium level. If you have a low level of potassium or a history of abnormal potassium levels, talk with your doctor before starting Xopenex or Xopenex HFA. These drugs can cause a temporary decrease in your potassium level, which may cause certain symptoms. See the section above called “Xopenex side effects” for more details.
- Problems with your blood sugar levels. If you have diabetes or other conditions that affect your blood sugar level, talk with your doctor before starting either Xopenex or Xopenex HFA. These medications may affect your blood sugar level. If you have diabetes or other conditions that affect your blood sugar, or if you’re taking other drugs that affect your blood sugar, your doctor may check your blood sugar level more often during treatment. This allows your doctor to see if Xopenex or Xopenex HFA is also affecting your blood sugar level.
- Pregnancy. It’s not known for sure if either Xopenex or Xopenex HFA is safe to use during pregnancy. For more information, please see the “Xopenex and pregnancy” section above.
- Breastfeeding. It’s not known for sure if either Xopenex or Xopenex HFA is safe to take while you’re breastfeeding. For more information, please see the “Xopenex and breastfeeding” section above.
Note: For more information about the potential negative effects of Xopenex, see the section “Xopenex side effects” above.
When you get Xopenex from the pharmacy, the pharmacist will add an expiration date to the label on the container. The expiration date helps guarantee the effectiveness of the medication during this time.
The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Storing Xopenex
Vials of Xopenex liquid solution come in a foil pouch. The vials should be stored between 68°F and 77°F (20°C and 25°C) and kept away from light and heat. Once you’ve opened the foil pouch holding each vial, the vial must be used within 2 weeks. If the vials are removed from the pouch before you’re ready to use them, they must be protected from light and used within 1 week.
Storing Xopenex HFA
Canisters of Xopenex HFA (aerosol spray) come in a box. The canisters should be stored between 68°F and 77°F (20°C and 25°C) and protected from direct sunlight. The mouthpiece of the inhaler should be facing down when it’s stored.
Do not puncture or burn canisters of Xopenex HFA. Also, avoid storing them near heat. If these canisters are exposed to temperatures above 120°F (49°C), they may burst open.
Disposal
If you no longer need to take Xopenex and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
The
Disposing of Xopenex
Vials containing Xopenex liquid solution should be thrown away if the solution inside the vials doesn’t appear clear and colorless.
Disposing of Xopenex HFA
Canisters containing Xopenex HFA should never be disposed of in a fire or incinerator. The medication inside the canisters is stored under pressure. If heated, the canisters may burst open.
The following information is provided for clinicians and other healthcare professionals.
Indications
Xopenex (levalbuterol hydrochloride) is:
- approved to treat or prevent bronchospasm in people ages 6 years and older with reversible obstructive airway disease
Xopenex HFA (levalbuterol tartrate) is:
- used to treat or prevent bronchospasm in people ages 4 years and older with reversible obstructive airway disease
Mechanism of action
Xopenex and Xopenex HFA are beta2 adrenergic-agonists, which activate receptors on the smooth muscle tissue of airways. This in turn activates adenylate cyclase to increase concentrations of cyclic adenosine monophosphate (AMP).
Increased concentrations of cyclic AMP activates protein kinase A, which interferes with the phosphorylation of myosin and decreases calcium concentrations in smooth muscle cells. This leads to relaxation in the muscles and provides relief of bronchospasm symptoms.
Xopenex and Xopenex HFA relax the airways from the trachea down to the terminal bronchioles. Because beta2-adrenergic receptors are also present in the heart, Xopenex may cause heart-related side effects.
Pharmacokinetics and metabolism
Peak concentrations of nebulized Xopenex are achieved within about 30 minutes in adults.
Xopenex and Xopenex HFA are metabolized in the gastrointestinal tract via sulfotransferase (SULT1A3) and are eliminated primarily in the urine as unchanged drug and metabolite. The elimination half-life of Xopenex is estimated to be 3 to 4 hours.
Contraindications
Xopenex and Xopenex HFA are contraindicated in people with a previous hypersensitivity reaction to levalbuterol or albuterol. Several different precautions exist. See additional information in the section “Xopenex precautions” above.
Storage
Storage instructions differ for Xopenex and Xopenex HFA. These instructions are described below.
Storing Xopenex
Vials containing Xopenex liquid solution are supplied in a foil pouch. This medication should be stored between 68°F and 77°F (20°C and 25°C), protected from light and heat. Once a foil pouch is opened, the vials must be used within 2 weeks. If vials are removed from the pouch, they must be protected from light and used within 1 week.
Storing Xopenex HFA
Canisters containing Xopenex HFA aerosol spray are supplied in a box. This medication should be stored between 68°F and 77°F (20°C and 25°C) and protected from direct sunlight. The actuator mouthpiece should be facing down when stored.
Do not puncture, burn, or store canisters near heat. Exposure to temperatures above 120°F (49°C) may cause bursting.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.