Tremfya is a brand-name prescription medication. It’s approved for use in adults to treat:
- Psoriatic arthritis. With psoriatic arthritis, you have psoriasis and pain and stiffness in your joints. For this use, Tremfya may be used alone or with certain other drugs.
- Moderate to severe plaque psoriasis. With plaque psoriasis, you have itchy patches on your skin. These may look pink or be darker than your skin color. Sometimes, they may look white and scaly. Plaque psoriasis is just one of many types of psoriasis. For this use, Tremfya may be an option if you can receive systemic therapy (medication that affects your whole body) or phototherapy (treatment with light).
Drug details
Tremfya contains the active drug guselkumab. It’s a biologic, which means that it’s made from parts of living organisms by using advanced technology. Tremfya belongs to a class of medications called interleukin-23 blockers. A class of drugs is a group of medications that work in a similar way.
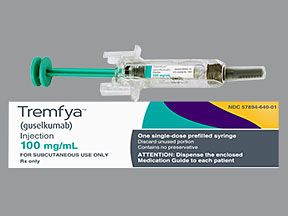
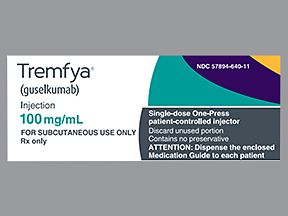
Tremfya comes as a liquid solution inside single-dose prefilled syringes and single-dose One-Press injectors. It’s available in one strength: 100 milligrams/milliliter.
The medication is given as an injection under your skin (a subcutaneous injection). A healthcare provider will give you your first dose of Tremfya. Then, they can show you or your caregiver how to give the injections at home.
FDA approval
In 2017, the Food and Drug Administration (FDA) approved Tremfya to treat moderate to severe plaque psoriasis in adults. Then later, in 2020, the FDA approved the drug to treat psoriatic arthritis.
Effectiveness
In clinical studies, Tremfya was effective in treating both psoriatic arthritis and plaque psoriasis. For information about these studies, see the “Tremfya for psoriatic arthritis” and “Other uses for Tremfya” sections below.
Tremfya contains the active drug guselkumab. It’s available only as a brand-name medication. Tremfya isn’t currently available in biosimilar form.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from parts of living organisms by using advanced technology. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Tremfya can cause mild or serious side effects. The following list contains some of the key side effects that may occur while taking Tremfya. This list does not include all possible side effects.
For more information on the possible side effects of Tremfya, or tips on how to deal with a troubling side effect, talk with your doctor or pharmacist.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs it has approved. If you would like to notify the FDA about a side effect you’ve had with Tremfya, you can do so through MedWatch.
More common side effects
The more common side effects of Tremfya can include:
- upper respiratory infections, including nose and throat infections such as the common cold
- injection site reactions (redness, swelling, or pain in the injection area)
- headaches
- joint pain
- diarrhea or gastroenteritis (stomach infection)
- higher levels of liver enzymes
- tinea (fungal) infections, such as jock itch and athlete’s foot
- herpes simplex infections, such as cold sores, fever blisters, and genital sores
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Tremfya aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or you think you’re having a medical emergency.
Serious side effects, explained in more detail below in “Side effect details,” include:
- allergic reactions
- tuberculosis (TB)
- infections
Side effect details
You may wonder how often certain side effects occur with this drug, or whether certain side effects pertain to it. Here’s some detail on some of the side effects this drug may or may not cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Tremfya. But it’s not known how many people have had an allergic reaction during Tremfya treatment.
Symptoms of a mild allergic reaction can include:
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, face, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Tremfya. But call 911 if your symptoms feel life threatening or you think you’re having a medical emergency.
Joint pain
You’re not likely to have joint pain while taking Tremfya. In one study of people with plaque psoriasis, only 2.7% of people who took Tremfya had joint pain. This was compared with 2.1% of people who took a placebo (treatment with no active drug). But keep in mind that psoriatic arthritis itself can also cause joint pain.
If you have joint pain that concerns you, talk with your doctor. They can suggest treatments to help you feel more comfortable.
Infections
Taking Tremfya may increase your risk for upper respiratory infections. This includes nose and throat infections. In clinical studies, 14.3% of people who took Tremfya had upper respiratory infections. This was compared with 12.8% of people who took a placebo (treatment with no active drug).
In a study of people with psoriatic arthritis, 1.6% to 2.9% of people taking Tremfya developed bronchitis (a type of respiratory tract infection). This was compared with 1.1% of people who took a placebo.
Upper respiratory infections are the same type of infection that causes cold symptoms. So if you have a runny or stuffy nose, cough, or sore throat, drink fluids and get plenty of rest. And if your symptoms are bothersome, talk with your doctor. They can suggest treatments to help you feel better.
Less common infections
It’s possible to develop other, less common infections while you’re taking Tremfya. But these infections are much less common than the upper respiratory infections mentioned above.
The less common infections include:
- fungal infections, such as athlete’s foot
- herpes infections, such as cold sores
Fungal or herpes infections occurred in 1.1% of people with plaque psoriasis who took Tremfya. This was compared with people who took a placebo (treatment with no active drug). In this group, 0% of people had a fungal infection and 0.5% of people had a herpes infection.
Fungal and herpes infections are easily treated, and you can ask your doctor or pharmacist for advice. But if these infections don’t go away within about a week or get worse, tell your doctor.
Injection site reaction
Taking Tremfya may cause you to have an injection site reaction. This is irritation near the spot where you had an injection. In clinical studies of people with plaque psoriasis, 4.5% of those who took Tremfya had injection site reactions. This was compared with 2.8% of people who took a placebo (treatment with no active drug). Symptoms included bruising, swelling, itching, and redness.
To help prevent injection site reactions, try injecting Tremfya in a different spot for each dose. Also, make sure you choose a spot that isn’t tender, scaly, red, or bruised. Follow the proper instructions on injections. (For more information, see the “How to take Tremfya” section below.) And keep in mind that it’s important to clean the injection site before an injection.
If your symptoms are bothering you, talk with your doctor. They may recommend a topical medication that you apply to your skin.
Tuberculosis
Before you take Tremfya, your doctor will likely check you for a type of lung infection called tuberculosis (TB). If you’ve had TB in the past, the infection could still be in your body without causing symptoms. Taking Tremfya could cause the TB to become active and bring on symptoms. It’s not known how many people had TB that became active while taking Tremfya.
It’s important to tell your doctor if you’ve ever had TB or have been treated for it. In these cases, your doctor may give you medication for TB before you start taking Tremfya. This may help prevent the TB infection from becoming active during your Tremfya treatment.
Symptoms of TB can include:
- cough
- extreme tiredness
- weight loss or loss of appetite
- night sweats
If you notice any of these symptoms while taking Tremfya, tell your doctor. They may pause your use of Tremfya to treat the TB.
Weight loss or weight gain (not a side effect)
Tremfya hasn’t been linked to weight loss or weight gain in studies. However, weight loss could be a sign of an infection, such as TB, or other condition that requires treatment. (For more about TB, see the “Tuberculosis” section right above.)
If you have unexpected weight loss or weight gain when taking Tremfya, tell your doctor. They can check to see what may be causing your weight to change.
Hair loss (not a side effect)
Taking Tremfya shouldn’t cause you to lose your hair. However, psoriasis of the scalp can lead to temporary hair loss. Using other psoriasis treatments (besides Tremfya) or having scalp irritation from scratching can also cause hair loss.
If you have psoriasis on your scalp and are concerned about losing your hair, talk with your doctor. They may be able to suggest ways to help prevent hair loss.
Fatigue (not a side effect)
Tremfya isn’t known to cause fatigue (lack of energy). However, fatigue could be a sign of an infection or other condition that requires treatment.
If you have fatigue while taking Tremfya, tell your doctor. They can look into possible causes.
Depression (not a side effect)
Depression isn’t a side effect of Tremfya. However, having plaque psoriasis or psoriatic arthritis may cause you to feel sad for periods of time. This sadness can vary depending on how severe your plaque psoriasis or psoriatic arthritis is. But as your condition improves, you may feel less discouraged, sad, and depressed.
If you’re concerned about depression, ask your doctor about a depression screening. And be sure to tell them if you’re feeling sad, irritable, or depressed. Many treatments are available to help you with these feelings.
The Tremfya dosage and dosing schedule your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Tremfya to treat
- other medical conditions you may have
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to suit your needs.
Drug forms and strengths
Tremfya comes as a solution that’s given as an injection under your skin (a subcutaneous injection). The medication is available in one strength: 100 milligrams/milliliter (mg/mL).
Tremfya comes in single-dose prefilled syringes and single-dose One-Press injectors. You may find one form easier to use than the other, so ask your doctor which form is right for you.
A healthcare provider will give you your first dose of Tremfya. Then they can show you or your caregiver how to give the injections at home.
Dosage for psoriatic arthritis
For psoriatic arthritis, your first dose of Tremfya will be a 100-mg injection. After 4 weeks, you’ll have another 100-mg injection. Then, you’ll have a 100-mg injection once every 8 weeks.
Note: If you’re using Tremfya for psoriatic arthritis, the drug may be taken alone or in combination with certain other drugs. These other drugs include certain disease-modifying antirheumatic drugs (DMARDs) such as methotrexate.
Dosage for plaque psoriasis
For plaque psoriasis, your first dose of Tremfya will be a 100-mg injection. After 4 weeks, you’ll have another 100-mg injection. Then, you’ll have a 100-mg injection once every 8 weeks.
What if I miss a dose?
If you miss a dose of Tremfya, take it as soon as you remember. Then take the next dose as originally scheduled. If you have questions about a missed dose, ask your doctor.
To help make sure that you don’t miss a dose, try putting your treatment schedule in a calendar. You can also set a reminder on your phone.
Will I need to use this drug long term?
Tremfya is meant to be used as a long-term treatment. If you and your doctor determine that Tremfya is safe and effective for you, you’ll likely take it long term.
As with all medications, the cost of Tremfya can vary. The actual price you’ll pay depends on your insurance coverage, location, and the pharmacy you use.
Financial and insurance assistance
If you need financial support to pay for Tremfya, or if you need help understanding your insurance coverage, help is available.
Janssen Biotech, Inc., the manufacturer of Tremfya, offers a program called Janssen CarePath. For more information and to find out if you’re eligible for support, call 877-227-3728 or view this program overview.
The Food and Drug Administration (FDA) approves prescription drugs such as Tremfya to treat certain conditions. In addition to treating psoriatic arthritis, which is discussed below, Tremfya is also approved for treating plaque psoriasis. For more information about this condition, see the “Other uses for Tremfya” section below.
When you have psoriatic arthritis, your immune system (your body’s defense against infections) is overactive. It attacks healthy tissues and cells, causing joint pain and inflammation. It also causes your body to make too many skin cells, leading to a buildup of cells and areas called plaques. These plaques are flushed, itchy patches on your skin.
For this condition, Tremfya may be taken alone or in combination with certain other drugs. These other drugs include certain disease-modifying antirheumatic drugs (DMARDs) such as methotrexate.
Effectiveness for psoriatic arthritis
Two clinical studies looked at adults with psoriatic arthritis who took either Tremfya or a placebo (treatment with no active drug). People’s responses to treatment were measured using the American College of Rheumatology’s (ACR) scoring system. With a score of ACR20, people had a 20% reduction in their psoriatic arthritis symptoms.
In the two studies, after 24 weeks of treatment, an ACR20 score was reached by:
- 52% to 64% of people who took Tremfya
- 22% to 33% of people who took the placebo
The Food and Drug Administration (FDA) approves prescription drugs such as Tremfya to treat certain conditions. In addition to treating plaque psoriasis, which is discussed below, Tremfya is also approved for treating psoriatic arthritis. For more information about this condition, see the “Tremfya for psoriatic arthritis” section above.
Tremfya may also be used off-label for other conditions, which are discussed below. (Off-label drug use is when a drug that’s approved to treat one condition is used to treat a different condition.)
Tremfya for plaque psoriasis
Tremfya is FDA-approved to treat moderate to severe plaque psoriasis. This condition is one of many types of psoriasis.
When you have plaque psoriasis, your immune system (your body’s defense against infections) is overactive. It causes your body to make too many skin cells, leading to a buildup of cells and areas called plaques. These plaques are itchy patches on your skin. They may look pink or be darker than your skin color. Sometimes, they may look white and scaly.
Tremfya may be an option for plaque psoriasis treatment if you can receive either:
- systemic therapy (treatment that affects your whole body), or
- phototherapy (treatment with light)
Effectiveness for plaque psoriasis
Clinical studies looked at adults with moderate to severe plaque psoriasis who took either Tremfya or a placebo (treatment with no active drug). After 16 weeks of treatment, psoriasis symptoms eased or cleared up entirely in:
- 84% to 85% of people who took Tremfya
- 7% to 8% of people who took the placebo
Tremfya for other conditions
In addition to the uses listed above, Tremfya may be used off-label for other uses. Off-label drug use is when a drug that’s approved for one use is used for a different one that’s not approved. And you may wonder if Tremfya is used for certain other conditions.
Tremfya for Crohn’s disease (off-label use)
Tremfya may be used off-label for the treatment of Crohn’s disease, which is a type of inflammatory bowel disease. Crohn’s disease can affect your digestive system, including your stomach, intestines, and colon. Janssen Biotech, Inc., the manufacturer of Tremfya, is currently studying Tremfya in people with Crohn’s disease.
Tremfya for ankylosing spondylitis (not an appropriate use)
Tremfya isn’t approved for the treatment of ankylosing spondylitis and shouldn’t be used off-label for this purpose. Ankylosing spondylitis is a type of arthritis (swelling in the joints) that affects your spine. Research doesn’t currently support the use of Tremfya for this condition.
Tremfya doesn’t interact with alcohol. But it’s important to consider how alcohol may affect your condition overall. Drinking alcohol may increase inflammation (swelling) in your body and make your plaque psoriasis or psoriatic arthritis worse. Alcohol may also make it harder for your immune system to fight off infections.
If you drink alcohol, talk with your doctor. They can tell you how much is safe for you to drink during your Tremfya treatment.
Other drugs are available that can treat psoriatic arthritis or plaque psoriasis. Some may be better suited for you than others. If you’re interested in finding an alternative to Tremfya, talk with your doctor to learn more about other medications that may work well for you.
Alternatives for psoriatic arthritis
Other medications that the Food and Drug Administration (FDA) has approved to treat psoriatic arthritis include:
- methotrexate
- adalimumab (Humira)
- etanercept (Enbrel)
- golimumab (Simponi)
- infliximab (Remicade, Renflexis, Inflectra)
Most of these medications are types of biologic drugs, which are made from parts of living organisms by using advanced technology. Biologic drugs affect your immune system in different ways to help treat psoriasis. (Your immune system is your body’s defense against infection.)
Alternatives for plaque psoriasis
Other medications that the FDA has approved to treat plaque psoriasis include:
- adalimumab (Humira)
- brodalumab (Siliq)
- certolizumab (Cimzia)
- etanercept (Enbrel)
- ixekizumab (Taltz)
- risankizumab (Skyrizi)
- secukinumab (Cosentyx)
- tildrakizumab (Ilumya)
- ustekinumab (Stelara)
- infliximab (Remicade, Renflexis, Inflectra)
These medications are all types of biologic drugs, which are made from parts of living organisms by using advanced technology. These drugs affect your immune system in different ways to help treat psoriasis. (Your immune system is your body’s defense against infection.)
You may wonder how Tremfya compares to other medications that are prescribed for similar uses. Here we look at how Tremfya and Stelara are alike and different.
Uses
The Food and Drug Administration (FDA) has approved both Tremfya and Stelara to treat:
- Psoriatic arthritis. With psoriatic arthritis, you have psoriasis and pain and stiffness in your joints. For this use, either drug may be used alone or in combination with certain other drugs.
- Moderate to severe plaque psoriasis. With plaque psoriasis, you have itchy patches on your skin. These may look pink or be darker than your skin color. Sometimes, they may look white and scaly. For this use, either drug may be an option if you can receive systemic therapy (medication that affects your whole body) or phototherapy (treatment with light).
Both Tremfya and Stelara can be used in adults. But Stelara is also approved for use in children ages 6 years and older.
In addition, Stelara is FDA-approved to treat Crohn’s disease and ulcerative colitis, which are types of inflammatory bowel disease.
Drug forms and administration
For psoriatic arthritis and plaque psoriasis, both Tremfya and Stelara are given as injections under your skin (subcutaneous injections). With either drug, a healthcare provider will administer your first dose. Then, they can show you or your caregiver how to give the drug at home.
For Tremfya
Tremfya comes as a solution inside single-dose prefilled syringes and single-dose One-Press injectors. You may find one form easier to use than the other, so ask your doctor which form is right for you.
After your first dose of the drug, you’ll receive another dose 4 weeks later. Then, you’ll receive another injection once every 8 weeks.
For Stelara
Stelara also comes as a solution. It’s available in single-dose prefilled syringes and single-dose vials.
After your first dose of the drug, you’ll receive another dose 4 weeks later. Then, you’ll receive another injection once every 12 weeks.
Side effects and risks
Tremfya and Stelara are both biologic drugs, which means that they’re made from parts of living organisms by using advanced technology. Therefore, both medications can cause some similar side effects. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Tremfya, with Stelara, or with both drugs (when taken individually).
- Can occur with Tremfya:
- joint pain
- Can occur with Stelara (when taken for psoriasis):
- myalgia (muscle pain)
- Can occur with both Tremfya and Stelara:
- upper respiratory infections, including nose and throat infections such as the common cold
- diarrhea or gastroenteritis (stomach infection)
- injection site reactions (redness, swelling, or pain in the injection area)
- infections caused by a fungus, such as athlete’s foot, or by the herpes virus, such as cold sores
Serious side effects
These lists contain examples of serious side effects that can occur with Tremfya, with Stelara, or with both drugs (when taken individually).
- Can occur with Tremfya:
- few unique serious side effects
- Can occur with Stelara:
- risk of certain infections including those of the skin, lungs, bones, and urinary tract
- a type of skin cancer called nonmelanoma
- reversible posterior leukoencephalopathy syndrome (a rare brain condition that’s usually curable with treatment)
- pneumonia that isn’t caused by an infection
- depression
- Can occur with both Tremfya and Stelara:
- allergic reaction
Effectiveness
Both Tremfya and Stelara are approved to treat plaque psoriasis and psoriatic arthritis.
The use of Tremfya and Stelara in treating moderate to severe plaque psoriasis has been directly compared in a clinical study. Researchers looked at people whose symptoms didn’t clear up within the first 16 weeks of Stelara treatment. These people then either took Stelara for 12 more weeks or took Tremfya for 12 weeks. Psoriasis symptoms cleared up entirely or eased in 31% of the people who took Tremfya. This was compared to 14% of people who took Stelara.
Costs
Tremfya and Stelara are both brand-name drugs. There are currently no biosimilar forms of either drug.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from parts of living organisms by using advanced technology. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Tremfya and Stelara generally cost about the same over time. The actual price you’ll pay for either drug depends on your insurance plan, location, and the pharmacy you use.
In addition to Stelara (discussed above), Humira is another drug that has a use similar to that of Tremfya. Here we look at how Tremfya and Humira are alike and different.
Uses
The Food and Drug Administration (FDA) has approved both Tremfya and Humira to treat:
- Psoriatic arthritis. With psoriatic arthritis, you have psoriasis and pain and stiffness in your joints. For this use, either drug may be used alone or in combination with certain other drugs.
- Moderate to severe plaque psoriasis. With plaque psoriasis, you have itchy patches on your skin. These may look pink or be darker than your skin color. Sometimes, they may look white and scaly. For this use, either drug may be an option if you can receive systemic therapy (medication that affects your whole body) or phototherapy (treatment with light).
Humira is also FDA-approved to treat the following conditions:
- rheumatoid arthritis, a type of arthritis can cause damage and joint pain throughout your body
- ankylosing spondylitis, a type of arthritis that affects your spine
- juvenile idiopathic arthritis, a type of arthritis in children
- Crohn’s disease in adults and children, a type of inflammatory bowel disease
- ulcerative colitis, a type of inflammatory bowel disease
- uveitis, a type of swelling in a part of your eye
- hidradenitis suppurativa, a type of painful skin condition
Tremfya is only approved for use in adults. Humira, on the other hand, is approved for use in children for some conditions.
Drug forms and administration
Both Tremfya and Humira are given as injections under your skin (subcutaneous injections). With either drug, a healthcare provider will administer your first dose. Then, they can show you or your caregiver how to give the drug at home.
For Tremfya
Tremfya comes as a solution inside single-dose prefilled syringes and single-dose One-Press injectors. You may find one form easier to use than the other, so ask your doctor which form is right for you.
After your first dose of the drug, you’ll receive another dose 4 weeks later. Then, you’ll receive another injection once every 8 weeks.
For Humira
Humira also comes as a solution. It’s available in single-dose prefilled syringes, single-dose prefilled pens, and single-use vials.
For psoriatic arthritis, after your first dose of the drug, you’ll receive another dose once every 2 weeks.
For plaque psoriasis, after your first dose of the drug, you’ll receive another dose 1 week later. Then, you’ll receive another injection once every 2 weeks.
Side effects and risks
Tremfya and Humiraare both biologic drugs, which means that they’re made from parts of living organisms by using advanced technology. Therefore, both medications can cause some similar side effects. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Tremfya, with Humira, or with both drugs (when taken individually).
- Can occur with Tremfya:
- diarrhea
- Can occur with Humira:
- nausea or abdominal (belly) pain
- high levels of cholesterol or lipids (fat-like molecules)
- blood in urine
- rash
- back pain
- urinary tract infection (UTI)
- high blood pressure
- Can occur with both Tremfya and Humira:
- upper respiratory infections, including nose and throat infections such as the common cold
- infections caused by a fungus, such as athlete’s foot, or by the herpes virus, such as cold sores
- injection site reaction (redness, swelling, or pain in the injection area)
- joint pain
Serious side effects
These lists contain examples of serious side effects that can occur with Tremfya, with Humira, or with both drugs (when taken individually).
- Can occur with Tremfya:
- few unique serious side effects
- Can occur with Humira:
- cancer such as lymphoma and a type of skin cancer* called nonmelanoma
- hepatitis B, if you’ve had it in the past
- demyelinating disease (a condition in which the coating of nerves is damaged) such as multiple sclerosis
- cytopenias (low blood cell counts)
- heart failure
- lupus-like syndrome (occurs when your immune system overreacts)
- Can occur with both Tremfya and Humira:
- allergic reaction
* Humira has a
Effectiveness
Both Tremfya and Humira are approved to treat plaque psoriasis and psoriatic arthritis.
The use of Tremfya and Humira in treating moderate to severe plaque psoriasis has been directly compared in a clinical study.
After 16 weeks, plaque psoriasis symptoms cleared up entirely or eased in 84% of people who took Tremfya. This was compared to 61% of people who took Humira. After 48 weeks, plaque psoriasis symptoms cleared up entirely or eased in 79% of people who took Tremfya. This was compared to 54% of people who took Humira.
The 2019 American Academy of Dermatology and the National Psoriasis Foundation guidelines recommend Humira as a treatment option for moderate to severe plaque psoriasis. Humira is taken more often than Tremfya, and you may be more likely to have side effects with Humira. Talk with your doctor about the treatment options that are best for you.
Costs
Tremfya and Humira are both brand-name drugs. Tremfya isn’t currently available in biosimilar form. But Humira has four biosimilars: Amjevita, Cyltezo, Hadlima, and Hyrimoz. They may cost less than Humira and Tremfya.
A biosimilar is a medication that’s similar to a brand-name drug. A generic medication, on the other hand, is an exact copy of a brand-name drug. Biosimilars are based on biologic medications, which are made from parts of living organisms by using advanced technology. Generics are based on regular medications, which are made from chemicals. Biosimilars and generics also usually cost less than brand-name drugs.
Tremfya and Humira generally cost about the same over time. The actual price you’ll pay for either drug depends on your insurance plan, location, and the pharmacy you use.
Tremfya is approved to treat psoriatic arthritis and plaque psoriasis in certain adults. For more information about these conditions, see the “Tremfya for psoriatic arthritis” and “Other uses for Tremfya” sections above.
What happens in psoriatic arthritis?
Psoriatic arthritis can occur when your immune system is extremely active. (Your immune system normally protects your body from infection.) But there are also other causes that trigger this condition. With psoriatic arthritis, you have both skin plaques (discussed below) and stiff or painful joints.
What happens in plaque psoriasis?
Plaque psoriasis can also occur when your immune system is extremely active. As a result, your body creates too many skin cells, which leads to buildup and inflammation (swelling). These skin cells form in hardened areas on your skin called plaques.
What Tremfya does
Tremfya belongs to a class of medications called biologics. These are made from parts of living organisms by using advanced technology. (A class of drugs is a group of medications that work in a similar way). Tremfya is also a monoclonal antibody, which is a type of protein that attaches to substances in the body. All monoclonal antibodies are considered to be biologics. Biologic drugs affect the body’s immune system in different ways depending on the drug.
Tremfya works by binding to interleukin-23 (a protein in the body) that’s overactive in people with plaque psoriasis or psoriatic arthritis. By binding to this protein, Tremfya decreases how active your immune system is to ease inflammation and help skin and joints heal.
How long does it take to work?
In clinical studies, people with plaque psoriasis saw results after taking three doses of Tremfya over 16 weeks. Researchers looked at adults with moderate to severe plaque psoriasis who took Tremfya or a placebo (treatment with no active drug). After 16 weeks, psoriasis symptoms cleared up entirely or eased in 84% to 85% of people who took Tremfya. This was compared with 7% to 8% of people who took a placebo.
In clinical studies, people with psoriatic arthritis also saw results after just 16 weeks of treatment. For instance, after this period of time, 52% to 55% of people taking Tremfya had a 20% reduction in their psoriatic arthritis symptoms. This was compared with 25% to 34% of people who took a placebo.
Tremfya can interact with several other medications. Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions increase the number of side effects or make them more severe.
Tremfya and other medications
Below is a list of medications that can interact with Tremfya. This list doesn’t contain all drugs that may interact with Tremfya.
Before taking Tremfya, be sure to tell your doctor and pharmacist about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Tremfya and the flu shot
Getting the nasal spray version of the flu vaccine (FluMist) while taking Tremfya may cause you to have an infection. This is because the nasal spray version of the flu shot is a live vaccine. Live vaccines contain a weakened form of a virus or bacteria. If your immune system (your body’s protection against infection) is healthy, live vaccines shouldn’t make you sick. But taking Tremfya may weaken your immune system. So your body may not be able to fight the virus or bacteria in the vaccine as your body usually would.
However, other forms of the flu vaccine that you receive as an injection may be safe for you to get. Ask your doctor which type of flu vaccine is right for you.
Tremfya and live vaccines
Getting live vaccines while taking Tremfya may cause you to have an infection. Live vaccines contain a weakened form of a virus or bacteria. If your immune system is healthy, live vaccines shouldn’t make you sick. But taking Tremfya may weaken your immune system. So your body may not be able to fight the virus or bacteria in the vaccine as your body usually would.
Examples of live vaccines that you should avoid include:
- yellow fever
- chickenpox
- nasal spray version of the flu vaccine (FluMist)
However, it’s safe to get non-live (inactive) vaccines during your Tremfya treatment. These vaccines don’t have any live viruses in them.
Before you start to take Tremfya, ask your doctor if you need any vaccines. It’s best to get these vaccines before you start your Tremfya treatment or get a non-live form while you take Tremfya.
Tremfya and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Tremfya. However, you should still check with your doctor or pharmacist before using any of these products while taking Tremfya.
You should take Tremfya according to your doctor or healthcare provider’s instructions.
Tremfya comes as a solution inside single-dose prefilled syringes and single-dose One-Press injectors. You may find one form easier to use than the other, so ask your doctor which form is right for you.
The medication is given as an injection just under your skin (a subcutaneous injection). A healthcare provider will usually give you your first dose. Then they can show you or your caregiver how to give injections at home. Also, the Tremfya website has instructions and videos to help you learn how to use Tremfya.
Take Tremfya out of the refrigerator to sit at room temperature for at least 30 minutes before each dose. This will help the injection feel more comfortable.
Be sure to look at the medication to make sure it’s not cloudy or discolored. If it is, dispose of the syringe or injector properly and use a new one.
After your injection, throw away the device and needle in an approved sharps container after use. (See the “Tremfya expiration, storage, and disposal” section below to learn more.)
Each prefilled syringe or One-Press injector holds only one dose. Don’t reuse either of them or try to give yourself more than one dose.
When to take
Your first dose of Tremfya will be a 100-mg injection. After 4 weeks, you’ll have another 100-mg injection. Then you’ll have a 100-mg injection once every 8 weeks.
To help make sure that you don’t miss a dose, try putting your treatment schedule on a calendar. You can also set a reminder on your phone.
It’s not known if Tremfya is safe to take during pregnancy. Studies into how Tremfya may affect pregnant people and their pregnancy aren’t available. But it’s thought that the drug may pass to a developing baby during pregnancy.
If you’re pregnant or want to become pregnant, talk with your doctor before taking Tremfya. They can discuss the pros and cons of the medication with you.
It’s not known if Tremfya is safe to take during pregnancy. So if you’re sexually active and you or your sexual partner can become pregnant, talk with your doctor about your birth control needs while you’re using Tremfya.
It’s not known if it’s safe to breastfeed while taking Tremfya. There are no studies of people who took Tremfya while breastfeeding. In animal studies, Tremfya didn’t pass through breast milk to breastfed offspring. But this doesn’t mean that the same result would occur in humans.
If you’re breastfeeding and interested in taking Tremfya, talk with your doctor. They can help you weigh the pros and cons of the medication.
Here are answers to some frequently asked questions about Tremfya.
How often will I need to have Tremfya injections?
After your first dose of Tremfya, you’ll have one dose 4 weeks later. Then you’ll have one dose of Tremfya every 8 weeks.
Tremfya comes as a solution inside prefilled syringes and One-Press injectors. The medication is given as an injection under your skin (a subcutaneous injection). A healthcare provider will give you your first dose. Then they can show you or your caregiver how to give injections at home.
If you have any questions about your treatment schedule, ask your doctor.
Will I still need to use topical skin treatments if I use Tremfya?
You might. Topical skin treatments are medications that you put on your skin. Your doctor may want you to use topical treatments with Tremfya if your plaque psoriasis or psoriatic arthritis skin lesions are severe. Or your doctor may want you to use a topical until Tremfya provides more relief on its own.
Some topical treatments for plaque psoriasis need to be prescribed by a doctor. But others are available without a prescription (over the counter).
Topical treatments that you get over the counter often include either salicylic acid or coal tar. Salicylic acid can help skin peel to lift psoriasis scales. And coal tar can help slow the growth of skin cells and ease itching.
You can also get mild topical corticosteroid creams over the counter, but higher-strength creams require a prescription. Corticosteroids can help ease inflammation (swelling).
If your symptoms are mild, you may only need topical treatment. But if your symptoms are moderate to severe, you may need an injectable medication such as Tremfya with a topical drug. Your doctor will work to create a medication plan that’s right for you.
If you have questions about any of your psoriasis medications, talk with your doctor or pharmacist.
Which vaccines aren’t safe to get while I’m taking Tremfya?
While you take Tremfya, avoid getting live (inactive) vaccines. These vaccines contain a weakened form of a virus or bacteria. If your immune system (your body’s protection against infection) is healthy, live vaccines shouldn’t make you sick. But taking Tremfya may weaken your immune system. So your body may not be able to fight the virus or bacteria in the vaccine as your body usually would.
Examples of live vaccines that you should avoid include:
- yellow fever
- chickenpox
- nasal spray version of the flu vaccine (FluMist)
However, it’s safe to get non-live (inactive) vaccines during your Tremfya treatment. These vaccines don’t have any live viruses in them. Examples of inactive vaccines include:
- flu shot (not the nasal spray)
- hepatitis A and hepatitis B vaccines
- pneumonia vaccine
Before you start to take Tremfya, ask your doctor if you need any vaccines. It’s best to get these vaccines before you start your Tremfya treatment or get a non-live form while you take Tremfya.
Can Tremfya cause cancer?
That’s not known for sure. In animal studies, researchers didn’t look to see if Tremfya increased the risk of cancer. In clinical trials of people taking the drug, cancer occurred in fewer than 1% of people.
If you have concerns about your risk for cancer while using Tremfya, talk with your doctor. They can discuss the risks and benefits of treatment with you.
Is Tremfya an immunosuppressant?
Yes, Tremfya is an immunosuppressant. This means that it works by lowering the activity of your immune system. (Your immune system normally protects your body from infection.)
Specifically, the drug binds to a certain protein in your body and decreases how active your immune system is. This action helps ease inflammation and reduce the symptoms of your condition.
If you have more questions about how this drug works, see the “How Tremfya works” section above.
Before taking Tremfya, talk with your doctor about your health history. Tremfya may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Infections. Taking Tremfya may make you more likely to develop an infection. This is because the drug may weaken your immune system (your body’s defense against infection). Your doctor will need to treat any infections you have before you can start taking Tremfya. If you develop symptoms of an infection (such as fever, extreme tiredness, or muscle aches) when taking Tremfya, tell your doctor.
- Tuberculosis. If you’ve had the lung infection tuberculosis (TB) in the past, taking Tremfya could make it active again and cause symptoms. So your doctor may give you medication for TB before you start taking Tremfya. They’ll likely test you for TB before you start Tremfya treatment. When taking Tremfya, tell your doctor if you have any possible symptoms of TB, such as extreme tiredness or a cough.
- Allergic reaction. If you’ve had an allergic reaction to Tremfya in the past, you shouldn’t take this drug. Tell your doctor about any medication allergies you have before starting treatment with Tremfya.
- Pregnancy. It’s not known whether Tremfya is safe to take during pregnancy. For more information, please see the “Tremfya and pregnancy” section above.
- Breastfeeding. It’s not known if it’s safe to breastfeed while taking Tremfya. For more information, please see the “Tremfya and breastfeeding” section above.
Note: For more information about the potential negative effects of Tremfya, see the “Tremfya side effects” section above.
Using more than the recommended dosage of Tremfya can lead to serious side effects. See the “Tremfya side effects” section above to learn more.
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor or seek guidance from the American Association of Poison Control Centers at 800-222-1222 or through their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Tremfya from the pharmacy, the pharmacist will add an expiration date to the label on the package. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee the effectiveness of the medication during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication. You should store Tremfya in its original packaging in the refrigerator at a temperature of 36°F to 46°F (2°to 8°C). It can only be out of the refrigerator at temperatures between 46°F and 86°F (8°C and 30°C) once for up to 4 hours before using.
Be sure to protect the drug from light. And don’t shake or freeze Tremfya.
Disposal
Tremfya syringes and injectors are made for single-use only. You’ll need to dispose of them in an approved sharps container after each injection. Don’t throw syringes, injectors, and needles away in the regular trash or recycling containers. This is because other people could get pricked by accident.
If you no longer need to take Tremfya and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children, from taking the drug by accident. Proper disposal also helps keep Tremfya from harming the environment.
The
The following information is provided for clinicians and other healthcare professionals.
Indications
Tremfya is indicated to treat psoriatic arthritis in adults. For this use, it may be used alone or in combination with certain disease-modifying antirheumatic drugs (DMARDs).
The drug is also indicated to treat moderate to severe plaque psoriasis in adults who are candidates for phototherapy or systemic therapy.
Mechanism of action
Tremfya is a human immunoglobulin G1 lambda (IgG1-lambda) monoclonal antibody and an interleukin-23 inhibitor. It attaches to the p19 subunit of interleukin-23 and blocks its receptor activity. This inhibits the release of inflammation-causing substances such as cytokines and chemokines and helps modulate the overactive immune response of plaque psoriasis and psoriatic arthritis.
Pharmacokinetics and metabolism
The precise mechanism of metabolism is currently unknown. In studies, peak serum concentrations were reached 5.5 days after administration of the drug. The average half-life of Tremfya is about 2 weeks (15 to 18 days).
Clinical studies indicate that clearance of Tremfya is not affected by age or weight, so dose adjustments do not appear to be necessary at this time. Studies to determine the impact of liver and kidney dysfunction on Tremfya metabolism and clearance are needed.
Contraindications
Tremfya is contraindicated in people who have had a serious allergic reaction to Tremfya or any of its ingredients in the past.
Storage
Tremfya should be protected from light and stored in the refrigerator 36 to 46°F (2 to 8°C). It should not be frozen or shaken. Prior to administration, it should be inspected for large particles, cloudiness, or discoloration.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up-to-date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.