Faslodex is a brand-name prescription medication that’s approved to treat certain types of breast cancer. Specifically, Faslodex is approved to treat hormone receptor-positive (HR+) breast cancer in the following ways:
- In postmenopausal women (they’ve already gone through menopause) with advanced breast cancer that got worse after previous hormone therapy. (This type of treatment works by blocking hormones that may be contributing to the growth of the cancer.)
- In postmenopausal women with HER2-negative (HER2–) advanced breast cancer who’ve never had hormone therapy before. (With HER2– cancer, the cancer cells don’t have abnormally high levels of a protein called HER2.)
- Along with ribociclib (Kisqali), in postmenopausal women with HER2– advanced or metastatic breast cancer who’ve never tried hormone therapy or whose breast cancer got worse after previous hormone therapy. (Metastatic cancer means it’s spread to other parts of the body.)
- Along with palbociclib (Ibrance) or abemaciclib (Verzenio), in women with HER2– advanced or metastatic breast cancer whose breast cancer got worse after hormone therapy.
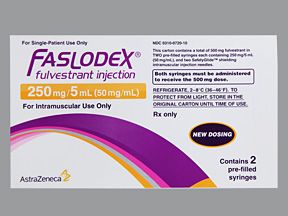
Faslodex contains the active drug fulvestrant. Faslodex is not approved for use in men or in children.
Faslodex is a type of hormone therapy. It works to block the amount of estrogen that your body produces. This helps stop cancer cells that depend on estrogen from growing and spreading.
Faslodex comes as a medication that’s injected into the muscle of your buttocks. You’ll receive Faslodex injections at your doctor’s office.
Effectiveness
In clinical trials, Faslodex was found to be effective at treating certain types of breast cancer. Faslodex was measured based on how many women had a complete or partial response to the drug. (A complete response is when there are no signs of breast cancer remaining after the medication is taken. A partial response is when the tumor decreases in size after the medication is taken.)
Faslodex was studied in postmenopausal women with HR+ breast cancer that had gotten worse after previous hormone therapy. This study compared Faslodex use with anastrozole (Arimidex) use. In this study, 17% of women taking Faslodex had a complete or partial response to the drug. Of the women taking anastrozole, 17% also had a complete or partial response to the drug.
For more information on Faslodex’s effectiveness, see the “Faslodex for breast cancer” section below.
Faslodex is available as a brand-name medication. It is also available in a generic form called fulvestrant.
A generic drug is an exact copy of the active drug in a brand-name medication. Generics tend to cost less than brand-name drugs.
Faslodex can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Faslodex. These lists do not include all possible side effects.
For more information on the possible side effects of Faslodex, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Faslodex, you can do so through MedWatch.
Mild side effects
The mild side effects of Faslodex 500 mg that are more common* can include:
- back pain
- fatigue (lack of energy)
- pain in the arms or legs
- hot flashes
- nausea
- bone pain
- joint pain
- pain at the injection site (See “Side effect details” below.)
- headache (See “Side effect details.”)
The mild side effects of Faslodex that are less common** can include:
- feeling weak
- vomiting
- constipation
- muscle pain
- cough
- diarrhea
- hair loss (See “Side effect details” below.)
- low appetite that can lead to weight loss (See “Side effect details.”)
- trouble breathing (See “Lung side effects” under “Side effect details.”)
* Occurred in 7% or more of people in clinical studies
** Occurred in less than 7% of people in clinical studies
Most of the side effects listed above are for a 500-mg dose of Faslodex when it’s taken alone. If you’re taking Faslodex along with other medications for your breast cancer, you may have side effects from those medications as well.
Most of these side effects may go away within a few days or a couple of weeks. But if they become more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Faslodex aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include:
- Elevated liver enzymes (the level of these enzymes in your blood shows how well your liver is working). Symptoms can include:
- abdominal (belly) pain
- jaundice (yellowing of your skin or the whites of your eyes)
- dark urine
- Bleeding. Symptoms can include:
- bruising easily
- bleeding that doesn’t easily stop after getting cut
- Allergic reaction. See “Side effect details” below.
Side effect details
You may wonder how often certain side effects occur with this drug or whether certain side effects pertain to it. Here’s some detail on several of the side effects this drug may or may not cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Faslodex. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing or speaking
It’s not known how many people in clinical trials had an allergic reaction to Faslodex. Call your doctor right away if you have a severe allergic reaction to Faslodex. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Weight gain or weight loss
Taking Faslodex may cause you to lose weight. This is because it can lower your appetite, which makes you not want to eat as much or as often.
Although a low appetite is a fairly common side effect, weight loss was not very common in clinical trials. The only clinical trial that weight loss was reported in was in a study of people taking Faslodex along with abemaciclib (Verzenio) or Faslodex and a placebo (a treatment with no active drug). In this study, 10% of women taking Faslodex with abemaciclib reported weight loss. In comparison, 2% of women taking Faslodex with a placebo reported a weight loss.
Weight gain is not a side effect that occurred in clinical trials. It’s unlikely that Faslodex will cause you to gain weight. Talk with your doctor if you’re concerned about your appetite or if you’re gaining or losing during your treatment.
Hair loss
Hair loss was a side effect seen in clinical trials in women taking Faslodex along with other drugs to treat their breast cancer. However, it was not reported as a common side effect in people taking Faslodex by itself to treat their breast cancer.
In clinical trials, 18% of women taking Faslodex with palbociclib (Ibrance) had hair loss. In comparison, 6% of women taking Faslodex and a placebo (a drug with no active drug) had hair loss.
In clinical trials, hair loss also occurred in about 16% of women taking Faslodex with abemaciclib (Verzenio). In comparison, 2% of women taking Faslodex and a placebo (a drug with no active drug), reported hair loss.
About 19% of women taking Faslodex and ribociclib (Kisqali) reported hair loss. In comparison, 5% of women taking Faslodex and a placebo (a treatment with no active drug) reported hair loss.
Talk with your doctor if you’re concerned about hair loss during your cancer treatment.
Injection site pain
Some people taking Faslodex may experience pain at the injection site. Because Faslodex is injected into the muscles of your buttock, it may cause pain in that area.
In clinical trials, injection site pain occurred in 11% of women taking Faslodex for hormone receptor-positive (HR+) breast cancer that got worse after previous hormone therapy. In comparison, 7% of women taking anastrozole (Arimidex) in this study had injection site pain from a placebo injection (an injection with no active drug).
There have also been reports of nerve damage related to the injection of Faslodex. Faslodex is injected into the buttocks, which is close to the sciatic nerve (a large nerve that travels from your spine into the back of your leg). Because of this, the injection could cause nerve pain or nerve damage to occur.
However, this was not a side effect that was commonly reported from women taking Faslodex in clinical trials. It’s not known how many people have experienced nerve damage from a Faslodex injection.
Talk with your doctor right away if you’re having severe injection site pain or a burning or shooting pain near the injection site.
Lung side effects
Some people may experience lung side effects while taking Faslodex. Lung side effects may include having trouble breathing or developing a cough or sore throat.
In clinical trials, 39% of women taking Faslodex for HR+ breast cancer that got worse after past hormone therapy reported having lung side effects. In comparison, 34% of women taking anastrozole (Arimidex) reported having lung side effects.
If you develop lung side effects such as trouble breathing, cough, or sore throat, talk with your doctor right away. They can recommend ways to help relieve this side effect.
Headache
Faslodex may cause headaches. In clinical trials, some people reported headache as a side effect of the medication. Of women taking Faslodex for HR+ breast cancer that got worse after previous hormone therapy, about 15% reported headaches. In comparison, about 17% of women taking anastrozole (Arimidex) reported headache as a side effect.
Talk with your doctor or pharmacist if you get headaches that are bothersome to you during your Faslodex treatment. They may be able to recommend pain relievers or other ways to help relieve your headaches.
The Food and Drug Administration (FDA) approves prescription drugs such as Faslodex to treat certain conditions. Faslodex may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Faslodex is approved to treat certain types of hormone receptor-positive (HR+) breast cancer in women. With HR+ breast cancer, the cancer is dependent on certain hormones, such as estrogen or progesterone, to grow and spread.
Faslodex is a hormone therapy that works by lowering the levels of these hormones in your body. When these hormone levels are reduced, HR+ breast cancers can’t grow as easily. This can help stop the spread of your cancer or get rid of it completely.
Faslodex for HR-positive, HER2-negative breast cancer
Faslodex is approved to treat HR+ breast cancer that’s HER2-negative (HER2–). This means the cancer cells don’t have abnormally high levels of a protein called HER2.
In women who haven’t had past treatments
If you’ve never had treatment for your HR+, HER2– breast cancer before, you can take Faslodex as your first treatment.
If your cancer is metastatic (has spread to other areas of your body), your doctor may have you start taking Faslodex and ribociclib (Kisqali) at the same time. In this case, Faslodex is only approved for use in postmenopausal women. (Postmenopausal women have already gone through menopause.)
In women whose past treatments didn’t work
If you have been treated for HR+, HER2– advanced or metastatic breast cancer before and your cancer got worse after hormone therapy, your doctor may have you start taking Faslodex. In this case, you’ll likely take Faslodex with palbociclib (Ibrance), abemaciclib (Verzenio), or ribociclib (Kisqali).
Faslodex for HR+ advanced breast cancer
Faslodex is also approved for use in postmenopausal women with advanced HR+ breast cancer who’ve tried hormone therapy before and whose breast cancer got worse after taking it. (Hormone therapy works by blocking hormones that may be contributing to the growth of the cancer.) In this case, Faslodex is used alone.
Effectiveness for breast cancer
In clinical trials, Faslodex was found to be effective at treating certain types of breast cancer. Faslodex was measured based on how many women had a complete or partial response to the drug. (A complete response is when there are no signs of breast cancer remaining after the medication is taken. A partial response is when the tumor decreases in size after the medication is taken.)
Effectiveness for HR+, HER2– breast cancer
Faslodex was studied in postmenopausal women with HR+, HER2– advanced or metastatic breast cancer who hadn’t tried hormone therapy before. This study compared Faslodex use with anastrozole (Arimidex) use. Of the women taking Faslodex, 46.1% had either a complete or partial response to the drug. In comparison, 44.9% of women taking anastrozole also had a complete or partial response to the drug.
Another clinical study looked at women with HR+, HER2– advanced breast cancer whose cancer got worse after previous hormone therapy. In the study, these women took either Faslodex with palbociclib (Ibrance) or Faslodex with a placebo (a treatment with no active drug). Of the women taking Faslodex with palbociclib, 24.6% had a complete or partial response to the drug. In comparison, 10.9% of women taking Faslodex and a placebo had a complete or partial response to the drug.
Faslodex was also studied in women with HR+, HER2– metastatic breast cancer whose cancer got worse after previous hormone therapy. These women took either Faslodex with abemaciclib (Verzenio) or Faslodex with a placebo (a treatment with no active drug). Of the women taking Faslodex with abemaciclib, 48.1% had a complete or partial response to the drug. In comparison, 21.3% of women taking Faslodex and a placebo had a complete or partial response to the drug.
Another clinical study looked at postmenopausal women with HR+, HER2– advanced breast cancer who had either never been treated for their breast cancer or whose breast cancer got worse after previous hormone therapy. Some women in the study took Faslodex with ribociclib (Kisqali), while others took Faslodex with a placebo.
Of the women who took Faslodex with ribociclib, 40.9% had a complete or partial response to the drug. In comparison, 28.7% of women taking Faslodex with a placebo had a complete or partial response to the drug.
Effectiveness for HR+ advanced breast cancer
Faslodex was studied in postmenopausal women with advanced HR+ breast cancer that had gotten worse after previous hormone therapy. This study compared Faslodex use with anastrozole (Arimidex) use. In this study, 17% of women taking Faslodex had a complete or partial response to the drug. Of the women taking anastrozole, 17% also had a complete or partial response to the drug.
Sometimes Faslodex is used along with other drugs to treat breast cancer. This is often done when cancer is metastatic (has spread to other parts of the body) and additional treatment is needed. It’s also done when the breast cancer is aggressive and needs to be treated with multiple medications at once to stop it from getting worse.
Faslodex is approved to be used with the following medications:
Faslodex with other drugs in premenopausal women
Faslodex is approved for use in women whose advanced or metastatic breast cancer is hormone receptor-positive (HR+) and HER2-negative (HER2–) and whose cancer got worse after previous hormone therapy. (This type of treatment works by blocking hormones that may be contributing to the growth of the cancer). Faslodex is approved for this use regardless of whether you’ve gone through menopause.
However, if you’re a premenopausal woman (haven’t started menopause yet) and you want to take Faslodex, you must also take a drug to lower the amount of estrogen your ovaries produce. (In premenopausal women, the ovaries are the main producers of estrogen.)
With HR+ breast cancer, more estrogen means the cancer grows more quickly. By blocking the large amounts of estrogen produced in a premenopausal woman’s ovaries, the cancer growth can be slowed or stopped completely.
Examples of medications that may be used to decrease estrogen produced by the ovaries include:
- leuprolide acetate (Lupron Depot)
- goserelin (Zoladex)
Use with Ibrance or Verzenio
Faslodex is approved for use with palbociclib (Ibrance) or abemaciclib (Verzenio) in women with HR+, HER2– advanced or metastatic breast cancer. It’s approved for this use if you’ve already tried hormone therapy and your cancer got worse.
Use with Kisqali
Faslodex is approved for use with ribociclib (Kisqali) in postmenopausal women with HR+, HER2– advanced or metastatic breast cancer. In this case, it can be used as the first hormone therapy you’ve tried or after you’ve tried another hormone therapy and your cancer got worse.
Faslodex is given as an injection by your doctor.
Injection site for Faslodex
Faslodex is injected into the muscle of your buttocks. Each dose is two injections. One syringe will be injected into your right buttock and the other into your left buttock. It’s a slow process that takes about 1 to 2 minutes per injection.
When to take
Faslodex is usually injected on days 1, 15, and 29 of your treatment. This means that for the first three doses, the injections are about 2 weeks apart. After that, you’ll only need to get Faslodex injections once a month.
To help make sure you don’t miss an appointment to get your Faslodex dose, try setting a reminder on your phone.
The Faslodex dosage your doctor prescribes may depend on other medical conditions you have.
Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, your doctor will determine the best dosage to fit your needs.
Drug forms and strengths
Faslodex comes as a medication that’s injected into the muscle of the buttocks. It’s available as a syringe that has 250 mg of Faslodex in 5 mL of solution. Usually, a dose of Faslodex is two syringes (500 mg total).
Dosage for breast cancer
Faslodex is given as an injection into the muscle of your buttocks. It will be given at your doctor’s office. Usually, you will receive two injections (one in each buttock muscle) each time you go for a dose of Faslodex. The usual dose is 500 mg (two injections of 250 mg).
Doses are taken on day 1, day 15, and day 29 in the first month. After the first three doses, you will only need Faslodex injections one time per month.
If you have other medical conditions such as liver failure, your doctor may decrease your dose of Faslodex. Talk to your doctor about any medical conditions that you have before starting Faslodex.
What if I miss a dose?
Faslodex is given as an injection by your doctor. Their office will work with you to make sure the injection appointments fit your schedule. To help make sure you don’t miss an appointment, try setting a reminder on your phone.
Will I need to use this drug long term?
Faslodex is meant to be used as a long-term treatment. It’s typically used until the cancer gets worse or spreads further. If you and your doctor determine that Faslodex is safe and effective for you, you’ll likely take it long term.
Other drugs are available that can treat hormone receptor-positive (HR+) breast cancer. Some may be a better fit for you than others. If you’re interested in finding an alternative to Faslodex, talk with your doctor. They can tell you about other medications that may work well for you.
Alternatives for HR-positive breast cancer
Following are examples of other drugs that may be used to treat HR+ breast cancer.
For postmenopausal women:
For premenopausal women:
- goserelin (Zoladex)
- leuprolide acetate (Lupron Depot)
- tamoxifen (Soltamox)
You may wonder how Faslodex compares with other medications that are prescribed for similar uses. Here we look at how Faslodex and Femara are alike and different.
Ingredients
The active drug ingredient in Faslodex is fulvestrant. The active drug ingredient in Femara is letrozole.
Uses
Faslodex is approved to treat hormone receptor-positive (HR+) breast cancer in the following ways:
- In postmenopausal women (they’ve already gone through menopause) with advanced breast cancer that got worse after previous hormone therapy. (This type of treatment works by blocking hormones that may be contributing to the growth of the cancer.)
- In postmenopausal women with HER2-negative (HER2–) advanced breast cancer who’ve never had hormone therapy before. (With HER2– cancer, the cancer cells don’t have abnormally high levels of a protein called HER2, which promotes cell growth.)
- Along with ribociclib (Kisqali), in postmenopausal women with HER2– advanced or metastatic breast cancer who’ve never tried hormone therapy or whose breast cancer got worse after previous hormone therapy. (Metastatic cancer means it’s spread to other parts of the body.)
- Along with palbociclib (Ibrance) or abemaciclib (Verzenio), in women with HER2– advanced or metastatic breast cancer whose breast cancer got worse after previous hormone therapy.
Femara is approved for use in postmenopausal women to:
- prevent HR+ early stage breast cancer from coming back after it’s been treated
- prevent early stage breast cancer from coming back after it’s been treated, after having taken tamoxifen (Soltamox) for 5 years
- treat HR+ (or unknown) advanced breast cancer as a first or second treatment
Drug forms and administration
Faslodex comes as a medication that’s injected into the muscle of the buttocks. You’ll receive Faslodex injections at your doctor’s office.
You’ll get Faslodex injections on days 1, 15, and 29 of your treatment. After the first three doses, you’ll get Faslodex injections once a month.
Femara is a tablet that’s taken by mouth. It’s usually taken once a day.
Side effects and risks
Faslodex and Femara have some similar side effects and others that differ. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Faslodex, with Femara, or with both drugs (when taken individually).
- Can occur with Faslodex:
- pain at the injection site
- back pain
- fatigue (lack of energy)
- pain in the arms or legs
- nausea
- vomiting
- constipation
- cough
- trouble breathing
- low appetite that can lead to weight loss
- diarrhea
- hair loss
- Can occur with Femara:
- flushing (warmth and redness in your skin)
- edema (fluid buildup in the body)
- dizziness
- high cholesterol
- excessive sweating
- Can occur with both Faslodex and Femara:
- hot flashes
- joint pain
- feeling weak
- headache
- bone pain
- muscle pain
Serious side effects
These lists contain examples of serious side effects that can occur with Faslodex or with Femara.
- Can occur with Faslodex:
- elevated liver enzymes (the level of these enzymes in your blood shows how well your liver is working)
- bleeding
- Can occur with Femara:
Effectiveness
These drugs haven’t been directly compared in clinical studies. However, studies have found both Faslodex and Femara to be effective for treating breast cancer.
A current clinical trial is testing the combination of palbociclib (Ibrance) and Femara compared with the combination of palbociclib and Faslodex. The study is comparing these medications in people with HR+, HER2– metastatic breast cancer. This study may help show which drug is a more effective option.
Another study showed that Femara and Faslodex can be used together in certain cases to treat metastatic breast cancer.
Costs
Faslodex and Femara are both brand-name drugs. There are currently generic forms of both drugs. Brand-name medications usually cost more than generics.
Faslodex costs significantly more than Femara. Generic Faslodex (fulvestrant) also costs significantly more than generic Femara (letrozole). The actual price you’ll pay for any of these drugs depends on your insurance plan, your location, and the pharmacy you use.
You may wonder how Faslodex compares with other medications that are prescribed for similar uses. Here we look at how Faslodex and Arimidex are alike and different.
Ingredients
The active drug ingredient in Faslodex is fulvestrant. The active drug ingredient in Arimidex is anastrozole.
Uses
Faslodex is approved to treat hormone receptor-positive (HR+) breast cancer in the following ways:
- In postmenopausal women (they’ve already gone through menopause) with advanced breast cancer that got worse after previous hormone therapy. (This type of treatment works by blocking hormones that may be contributing to the growth of the cancer.)
- In postmenopausal women with HER2-negative (HER2–) advanced breast cancer who’ve never had hormone therapy before. (With HER2– cancer, the cancer cells don’t have abnormally high levels of a protein called HER2, which promotes cell growth.)
- Along with ribociclib (Kisqali), in postmenopausal women with HER2– advanced or metastatic breast cancer who’ve never tried hormone therapy or whose breast cancer got worse after previous hormone therapy. (Metastatic cancer means it’s spread to other parts of the body.)
- Along with palbociclib (Ibrance) or abemaciclib (Verzenio), in women with HER2– advanced or metastatic breast cancer whose breast cancer got worse after previous hormone therapy.
Arimidex is approved for use in postmenopausal women to:
- prevent HR+ early stage breast cancer from returning after it’s been treated
- treat HR+ (or unknown) metastatic or locally advanced breast cancer as the first treatment option (locally advanced means the cancer has spread only to areas close by, such as the skin or surrounding lymph nodes)
- treat advanced breast cancer in women whose cancer got worse after tamoxifen (Soltamox) treatment*
* Breast cancer that’s HR-negative or that didn’t respond to tamoxifen treatment usually does not respond to Arimidex.
Drug forms and administration
Faslodex comes as a medication that’s injected into the muscle of the buttocks. You’ll receive Faslodex injections at your doctor’s office.
You’ll get Faslodex injections on days 1, 15, and 29 of your treatment. After the first three doses, you’ll get Faslodex injections once a month.
Arimidex comes as an oral tablet that’s taken once a day.
Side effects and risks
Faslodex and Arimidex have some similar side effects and others that vary. Below are examples of these side effects.
Mild side effects
These lists contain examples of mild side effects that can occur with Faslodex, with Arimidex, or with both drugs (when taken individually).
- Can occur with Faslodex:
- pain at the injection site
- fatigue (lack of energy)
- pain in the arms or legs
- bone pain
- constipation
- muscle pain
- low appetite that can lead to weight loss
- diarrhea
- hair loss
- Can occur with Arimidex:
- throat pain
- high blood pressure
- depression
- rash
- osteoporosis
- bone fractures
- insomnia (trouble sleeping)
- swelling of the arms or legs
- swollen lymph nodes
- Can occur with both Faslodex and Arimidex:
- hot flashes
- feeling weak
- joint pain
- nausea
- vomiting
- back pain
- headache
- cough
- trouble breathing
Serious side effects
These lists contain examples of serious side effects that can occur with Faslodex or with Arimidex.
- Can occur with Faslodex:
- elevated liver enzymes (the level of these enzymes in your blood shows how well your liver is working)
- bleeding
- Can occur with Arimidex:
Effectiveness
Faslodex and Arimidex have different FDA-approved uses, but they’re both used to treat certain types of breast cancer.
In a clinical study, Faslodex was compared with anastrozole (Arimidex) for treating postmenopausal women with HR+, HER2– breast cancer. This study specifically looked at women with locally advanced or metastatic breast cancer who had never been treated for their breast cancer before.
Faslodex was measured by showing how many women had a complete or partial response to the drug. (A complete response is when there are no signs of breast cancer remaining after the medication is taken. A partial response is when the tumor decreases in size after the medication is taken.)
In this study, 46.1% of women taking Faslodex had either a complete or partial response. In comparison, 44.9% of women taking anastrozole had a complete or partial response.
Faslodex was also studied in postmenopausal women with HR+ breast cancer that had gotten worse after previous hormone therapy. This study compared Faslodex use with anastrozole use. In this study, 17% of women taking Faslodex had a complete or partial response to Faslodex. Of the women taking anastrozole, 17% also had a complete or partial response to Faslodex.
Costs
Faslodex and Arimidex are both brand-name drugs. There are currently generic forms of both drugs. Brand-name medications usually cost more than generics.
Faslodex costs significantly more than Arimidex. The generic form of Faslodex (fulvestrant) also costs significantly more than the generic form of Arimidex (anastrozole). The actual price you’ll pay for either drug depends on your insurance plan, your location, and the pharmacy you use.
Here are answers to some frequently asked questions about Faslodex.
Will I need to take other medications with Faslodex to treat or prevent bone problems?
Yes. Usually, people taking Faslodex should also take a medication to prevent
In addition, medications used to treat your breast cancer will further lower your estrogen levels. This may increase your risk for bone loss. Medications such as zoledronic acid (Zometa) may be used along with Faslodex to prevent bone loss.
You may also need to take another medication if your breast cancer has spread into your bones. Denosumab (Xgeva) is used with chemotherapy to prevent and treat several types of bone problems in people with cancer.
Talk with your doctor about taking a medication to treat or prevent bone problems while you’re taking Faslodex.
Can Faslodex be used by men with breast cancer?
No, Faslodex is not approved for use in men with breast cancer. It’s not known if Faslodex is safe and effective for men with breast cancer because it hasn’t been studied in men.
Approved treatments for men with breast cancer include tamoxifen (Soltamox) and palbociclib (Ibrance). However, your doctor may use Faslodex off-label to treat breast cancer in men. (Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.)
Talk with your doctor about the best way to treat your breast cancer.
Is Faslodex a chemotherapy drug?
No, Faslodex is not a chemotherapy drug. It’s a hormone therapy that works by decreasing the levels of certain hormones (estrogen and progesterone) in your body. These hormones cause your hormone receptor-positive (HR+) cancer to grow, so blocking them can help stop the spread of cancer or get rid of it completely.
I’ve had a mastectomy — can I take Faslodex?
Yes, you can still take Faslodex if you’ve had a mastectomy (surgery to remove breast tissue). Even if your cancer didn’t spread outside the breast tissue, it’s still possible that some cancer cells escaped into your blood or lymph nodes. This can cause problems later on.
Faslodex lowers the amount of estrogen in your body, which stops HR+ tumor cells from growing and multiplying. Taking Faslodex after a mastectomy helps lower your risk of the cancer spreading or coming back.
If I haven’t gone through menopause yet, will Faslodex affect my periods?
Yes, Faslodex may affect your periods if you haven’t gone through menopause yet. This is because Faslodex changes your hormone levels.
Faslodex decreases estrogen and progesterone levels in your body. These hormones are very important to the menstrual cycle. They help you ovulate, which causes your period to occur a few weeks later. Because your hormone levels will be affected, your period may become irregular or infrequent. In some women, it may stop completely.
Talk with your doctor if you have concerns about how Faslodex will affect your period.
The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
It’s important to note that you’ll have to get Faslodex at a specialty pharmacy. This type of pharmacy is authorized to carry specialty medications. These are drugs that may be expensive or may require help from healthcare professionals to be used safely and effectively.
Your insurance plan may require you to get prior authorization before approving coverage for Faslodex. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug. The insurance company will review the request and let you and your doctor know if your plan will cover Faslodex.
If you’re not sure if you’ll need to get prior authorization for Faslodex, contact your insurance plan.
Financial and insurance assistance
If you need financial support to pay for Faslodex, or if you need help understanding your insurance coverage, help is available.
AstraZeneca, the manufacturer of Faslodex, offers a program called Access 360, which can help answer your questions about the cost of this drug. The manufacturer also offers the Faslodex Patient Savings Program, which can help lower the cost of the drug.
For more information about these programs, visit the manufacturer’s website.
Faslodex is approved to treat breast cancer that’s hormone receptor-positive (HR+).
What happens in HR+ breast cancer
Breast cancer occurs when you develop a tumor in your breast from cells growing too quickly and out of control. With HR+ breast cancer, the cancer is dependent on hormones, such as estrogen or progesterone, to grow and spread.
Estrogen causes two enzymes (a type of protein) within the cancer cells to become overactive. These enzymes are called cyclin-dependent kinases 4 and 6 (CDK 4 and 6).
CDK 4 and 6 help regulate how all cells grow and multiply. When they become overactive in cancer cells, they make the cancer cells grow and spread more rapidly.
What Faslodex does
Faslodex works by blocking estrogen from attaching to the estrogen receptors (docking stations) on your cells. Faslodex attaches itself to the receptors so that there isn’t a place for estrogen to attach to the cells. This prevents estrogen from stimulating the cancer cells to grow and multiply.
How long does it take to work?
It can take about 1 month (your first three doses) for Faslodex to begin effectively treating your breast cancer. You won’t be able to feel the effects of Faslodex in your body. However, your doctor should do tests during your treatment to check whether Faslodex is working for you.
There are no known interactions between Faslodex and alcohol.
However, if you have alcoholic liver disease (or liver disease from another cause), you may have to take a lower dose of Faslodex. This is because the normal dose may cause Faslodex to build up in your body.
If you drink alcohol, talk with your doctor about how much is safe to drink while you’re taking Faslodex.
Faslodex is not known to interact with any medications. It’s also not known to interact with any supplements or foods. However, Faslodex can affect the results of certain lab tests.
Faslodex and other medications
There are no medications that are known to interact with Faslodex. However, it’s still important to go over the medications you’re taking with your doctor before starting Faslodex.
Before taking Faslodex, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Faslodex and herbs and supplements
There aren’t any herbs or supplements that have been specifically reported to interact with Faslodex. However, you should still check with your doctor or pharmacist before using any of these products while taking Faslodex.
Faslodex and foods
There aren’t any foods that have been specifically reported to interact with Faslodex. If you have any questions about eating certain foods with Faslodex, talk with your doctor.
Faslodex and lab tests
Faslodex can affect the measurement of estrogen in your blood. This is because Faslodex is very similar to estrogen. Taking Faslodex can cause results from an estrogen blood test to be falsely high.
Estrogen can also be measured by urine tests or saliva tests. If you’re taking Faslodex and your doctor needs to check your estrogen levels, they may use a urine or saliva test (which aren’t affected by Faslodex) instead of a blood test.
Faslodex is not safe to take during pregnancy. This drug hasn’t been studied in pregnant women. However, in animal studies of females taking Faslodex, fetuses had problems with bone growth and skeleton formation. Pregnant females also had a higher risk of miscarriage.
Because of this risk of harm to a fetus, you should use an effective method of birth control while taking Faslodex and for 1 year after your last dose of Faslodex.
If you are pregnant or planning to become pregnant, talk with your doctor before starting Faslodex. They will likely recommend a different treatment option for you.
It’s not safe to take Faslodex during pregnancy. If you’re sexually active and can become pregnant, talk with your doctor about your birth control needs while you’re using Faslodex.
You should take a pregnancy test within 7 days before starting Faslodex. You’ll need to use birth control while taking Faslodex and for 1 year after your last dose.
In most cases, you shouldn’t breastfeed while taking Faslodex and for 1 year after your last dose. It’s not known if Faslodex is safe to take while breastfeeding and whether it passes into breastmilk. However, in animal studies, Faslodex was present in the milk of lactating animals.
If you are currently breastfeeding or have other questions, talk with your doctor.
Before taking Faslodex, talk with your doctor about your health history. Faslodex may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Bleeding disorders. If you have any bleeding disorders, such as thrombocytopenia (low levels of platelets), talk with your doctor before starting Faslodex. You should also tell your doctor if you have a higher risk for bleeding because you take an anticoagulant (blood thinner). Faslodex is injected into your muscle, and if you have a bleeding disorder, your blood may not clot properly after the injection. This may raise your risk for bleeding. Tell your doctor about any medical conditions or medications you take before starting Faslodex.
- Pregnancy. It’s not safe to take Faslodex during pregnancy. You should use birth control while taking Faslodex and for 1 year after your last dose. For more information, see the “Faslodex and pregnancy” section above.
- Breastfeeding. In most cases, you shouldn’t breastfeed while taking Faslodex or for 1 year after your last dose. For more information, see the “Faslodex and breastfeeding” section above.
- Allergic reaction. If you’ve ever had an allergic reaction to Faslodex or any of the ingredients in Faslodex, you should not take this drug. Talk with your doctor about other treatment options for your breast cancer.
Note: For more information about the potential negative effects of Faslodex, see the “Faslodex side effects” section above.
The following information is provided for clinicians and other healthcare professionals.
Indications
Faslodex is approved to treat hormone receptor-positive (HR+) breast cancer:
- in postmenopausal women whose breast cancer got worse after previous hormone therapy
- in postmenopausal women with HER2-negative (HER2–) advanced breast cancer who had never been treated with hormone therapy before
- in combination with ribociclib (Kisqali), in postmenopausal women with HER2– advanced or metastatic breast cancer who have never tried hormone therapy or whose breast cancer got worse after previous hormone therapy
- in combination with palbociclib (Ibrance) or abemaciclib (Verzenio), in women with HER2– advanced or metastatic breast cancer whose breast cancer got worse after previous hormone therapy
Faslodex is not approved for use in men or in children.
Mechanism of action
Faslodex is a type of hormone therapy that works by binding to and therefore blocking the estrogen receptor. Once Faslodex is bound to the estrogen receptor, estrogen can no longer bind to it and cannot cause the growth or spread of cancer cells mediated by estrogen.
Faslodex may also be effective at blocking the spread of tamoxifen-resistant breast cancer in addition to breast cancer that is sensitive to estrogen.
Pharmacokinetics and metabolism
Faslodex approaches steady state after about the first month of treatment. The dosing is about every 2 weeks for the first three doses (days 1, 15, and 29), and then changes to once monthly after the drug has reached steady state.
Faslodex is about 99% plasma protein bound. Due to the similarities between Faslodex and endogenous estrogen, Faslodex is also believed to be metabolized via biotransformation (oxidation, hydroxylation, or conjugation) just as endogenous estrogen is. Cytochrome P-450 enzymes do not appear to be involved in the metabolism with the exception of CYP3A4, which plays a role in oxidation of Faslodex.
Faslodex is mainly cleared through the feces. Less than 1% of the drug is cleared renally. The half-life of Faslodex is about 40 days.
Contraindications
Faslodex is contraindicated in patients who have had a hypersensitivity reaction to it or any of its components in the past.
Storage
Faslodex should be stored in the refrigerator, between 36°F to 46°F (2°C to 8°C). It should be protected from light by keeping it in the original carton until you are ready to administer the dose.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.