Bosulif is a brand-name prescription medication. It’s FDA-approved for use in adults with a certain type of blood cancer called Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML). CML is also referred to as chronic myelogenous leukemia.
Bosulif is used for Ph+ CML in two ways:
- to treat newly diagnosed Ph+ CML*
- to treat Ph+ CML in people who’ve tried a previous treatment that either didn’t work or caused side effects that required stopping treatment
Bosulif contains the drug bosutinib, which belongs to a class of drugs called tyrosine kinase inhibitors (TKIs).
Bosulif comes as a tablet that you take by mouth once a day with food.
* For this use, Bosulif received
Effectiveness
For information about Bosulif’s effectiveness, see the “Bosulif uses” section.
Bosulif is available only as a brand-name medication. It’s not currently available in generic form.
A generic drug is an exact copy of a brand-name medication. Generics tend to cost less than brand-name drugs.
Bosulif contains the active drug bosutinib.
Bosulif can cause mild or serious side effects. The following lists contain some of the key side effects that may occur while taking Bosulif. These lists do not include all possible side effects.
For more information on the possible side effects of Bosulif, talk with your doctor or pharmacist. They can give you tips on how to deal with any side effects that may be bothersome.
Note: The Food and Drug Administration (FDA) tracks side effects of drugs they have approved. If you would like to report to the FDA a side effect you’ve had with Bosulif, you can do so through MedWatch.
More common side effects
The more common side effects of Bosulif can include:
- nausea or vomiting
- abdominal (belly) pain
- fatigue (lack of energy)
- rash
- fever
- flu
- shortness of breath
- coughing
- headache
- low appetite
- edema (fluid buildup in your body)
- diarrhea (See “Side effect details” below.)
Most of these side effects may go away within a few days or a couple of weeks. If they’re more severe or don’t go away, talk with your doctor or pharmacist.
Serious side effects
Serious side effects from Bosulif aren’t common, but they can occur. Call your doctor right away if you have serious side effects. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Serious side effects and their symptoms can include the following:
- Gastrointestinal toxicity (severe stomach problems). Symptoms can include:
- severe diarrhea
- severe vomiting
- low appetite
- severe abdominal (belly) pain
- Kidney damage or kidney failure. Symptoms can include:
- urinating less often than usual
- edema (water retention leading to swelling of legs, ankles, and feet)
- fatigue (lack of energy)
- nausea
- confusion
- hypertension (high blood pressure)
- Severe fluid retention (buildup) in and around the heart, lungs, and abdomen (belly). Symptoms can include:
- unexpected, rapid weight gain
- chest pain
- shortness of breath
- trouble breathing when you lie down
- swollen abdomen (belly)
Other serious side effects are discussed in the “Side effect details” section below. These include:
- liver damage
- heart failure
- blood disorders, including thrombocytopenia (low levels of platelets), anemia (low level of red blood cells), and neutropenia (low levels of white blood cells)
Side effect details
You may wonder how often certain side effects occur with this drug. Here’s some detail on several of the side effects this drug may cause.
Allergic reaction
As with most drugs, some people can have an allergic reaction after taking Bosulif. Symptoms of a mild allergic reaction can include:
- skin rash
- itchiness
- flushing (warmth and redness in your skin)
A more severe allergic reaction is rare but possible. Symptoms of a severe allergic reaction can include:
- swelling under your skin, typically in your eyelids, lips, hands, or feet
- swelling of your tongue, mouth, or throat
- trouble breathing
Call your doctor right away if you have a severe allergic reaction to Bosulif. Call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Diarrhea
Like many other drugs used for cancer, Bosulif may cause diarrhea in some people. In clinical studies, about 70% to 85% of people taking Bosulif had diarrhea. Of those people, 8% to 9% had severe diarrhea (seven or more stools per day and difficulty controlling their bowel movements).
In these studies, people taking Bosulif had diarrhea that started 2 to 3 days after they began taking Bosulif, and it lasted about 2 to 3 days total. For most people, this side effect gets better over time. However, some people experienced more frequent and longer episodes of diarrhea.
If you have diarrhea while taking Bosulif or other medications, talk with your doctor about how to manage this side effect.
But call your doctor right away if you become dizzy, dehydrated, or see blood or black spots in your stool. And call 911 if your symptoms feel life threatening or if you think you’re having a medical emergency.
Liver damage
Taking Bosulif may cause liver damage. This damage is most commonly found when doctors monitor enzymes (a type of protein) made in the liver. Enzyme levels that are higher than usual can be a sign of liver damage.
In clinical studies, 15% to 31% of people taking Bosulif had enzyme levels that were higher than usual. This typically happened within the first 3 months of taking Bosulif. After that, enzyme levels went back to normal in most people.
Some physical symptoms of liver damage include:
- nausea
- diarrhea
- loss of appetite
- itchy skin
- jaundice (yellowish color of your skin and whites of your eyes)
- edema (fluid buildup in your body)
- frequent bruising
- frequent bleeding
- ascites (fluid buildup in your belly)
During the first 3 months that you take Bosulif, your doctor may perform monthly enzyme tests to monitor your liver.
Heart failure
Taking Bosulif may cause heart failure. Heart failure was more common in people who’ve tried a previous treatment compared with people who were newly diagnosed. People who had heart failure were more likely to be older and had risk factors, such as a history of previous heart failure.
In a clinical study of people newly diagnosed with Ph+ CML, 1.5% of people taking Bosulif had heart failure. In another clinical study of people who were previously treated for Ph+ CML, 5.3% of people taking Bosulif had heart failure.
Some physical symptoms of liver damage include:
- trouble breathing
- swelling in your arms or legs
- fatigue (lack of energy)
- sudden weight gain
- heart palpitations (fast or fluttering heartbeat)
Your doctor may monitor you for signs of heart failure while you’re taking Bosulif. If needed, your doctor may change or stop your dose of Bosulif.
Blood disorders
Bosulif use may cause blood disorders, including thrombocytopenia (low levels of platelets), anemia (low levels of red blood cells), or neutropenia (low levels of white blood cells).
In clinical studies of people taking Bosulif:
- Up to 14.2% of people newly diagnosed and up to 34% of people previously treated had low levels of platelets.
- Up to 9% of people newly diagnosed and up to 22% of people previously treated had low levels of white blood cells.
- Up to 7.1% of people newly diagnosed and up to 19% of people previously treated had low levels of red blood cells.
Some physical symptoms of blood disorders can include:
- fatigue
- rapid heart rate
- shortness of breath
- frequent infections
- fevers
- bleeding gums
- blood in urine or stool
Your doctor will run tests to monitor your blood while you’re taking Bosulif. Based on your blood cell levels, your doctor may change your Bosulif dosage or ask you to temporarily stop taking it.
As with all medications, the cost of Bosulif can vary. The actual price you’ll pay depends on your insurance plan, your location, and the pharmacy you use.
Your insurance plan may require you to get prior authorization before approving coverage for Bosulif. This means that your doctor and insurance company will need to communicate about your prescription before the insurance company will cover the drug.
The insurance company will review the request and let you and your doctor know if your plan will cover Bosulif.
If you’re not sure if you’ll need to get prior authorization for Bosulif, contact your insurance company.
Financial and insurance assistance
If you need financial support to pay for Bosulif, or if you need help understanding your insurance coverage, help is available.
Pfizer Inc., the manufacturer of Bosulif, offers a program called Pfizer Oncology Together. For more information and to find out if you’re eligible for support, call 877-744-5675 or visit the program website.
The Bosulif dosage your doctor prescribes will depend on several factors. These include:
- the type and severity of the condition you’re using Bosulif to treat
- any side effects you have while taking Bosulif
- your age
- other medical conditions you may have
Typically, your doctor will start you on a low dosage. Then they’ll adjust it over time to reach the amount that’s right for you. Your doctor will ultimately prescribe the smallest dosage that provides the desired effect.
The following information describes dosages that are commonly used or recommended. However, be sure to take the dosage your doctor prescribes for you. Your doctor will determine the best dosage to fit your needs.
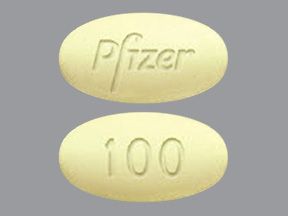
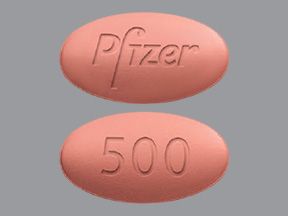
Drug forms and strengths
Bosulif comes as a tablet taken by mouth. It’s available in three strengths: 100 mg, 400 mg, and 500 mg.
Dosage for Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML)
For adults with Ph+ CML, there are two possible dosages.
- For people with newly diagnosed Ph+ CML who haven’t taken any other cancer drugs yet, the dosage is 400 mg once daily with food.
- For those who have tried another medication that either didn’t work or caused negative side effects, the dosage is 500 mg once daily with food.
In some cases, your doctor may start you at a lower dose and increase your dose by 100 mg every day until a maximum dose of 600 mg is reached.
If you experience certain side effects or have a blood, liver, or kidney disorder, your doctor may adjust your dose.
What if I miss a dose?
If you miss a dose, take it as soon as you remember. However, if it’s been more than 12 hours since your last dose, just skip the missed dose and take your regular dose the next day. Never take two doses to make up for a missed dose. This can raise your risk for serious side effects.
To help make sure you don’t miss a dose, try setting a reminder on your phone. A medication timer may be useful, too.
Will I need to use this drug long term?
Bosulif is meant to be used as a long-term treatment. If you and your doctor determine that Bosulif is safe and effective for you, you’ll likely take it long term.
The Food and Drug Administration (FDA) approves prescription drugs such as Bosulif to treat certain conditions. Bosulif may also be used off-label for other conditions. Off-label use is when a drug that’s approved to treat one condition is used to treat a different condition.
Bosulif for Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML)
The Food and Drug Administration (FDA) has approved Bosulif to treat a blood cancer called Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in adults. CML is also referred to as chronic myelogenous leukemia. Bosulif works by stopping or slowing down the growth of cancer cells.
Effectiveness for newly diagnosed Ph+ CML
Bosulif has been found to be effective in treating newly diagnosed Ph+ CML in people who haven’t received treatment for their cancer before. For this use, Bosulif received
This ongoing clinical trial compares Bosulif and imatinib (Gleevec) in people who were diagnosed with Ph+ CML and haven’t received treatment for their cancer before. The study is set to continue for up to 5 years before there are final results, but some results were reported after the first year.
Bosulif’s and Gleevec’s effectiveness is measured with bone marrow tests. These tests take bone marrow samples and count the number of cells that remain in the body after treatment. In this clinical trial, responses were reported as major molecular response (MMR) and complete cytogenetic response (CCyR). MMR tests bone marrow at the genetic level. This is more specific than CCyR, which tests it at the cellular level.
MMR means the level of cells with the BCR-ABL gene (the mutation that causes chromosomes to be Ph+) was at least 1,000 times less than the levels of a person with CML who was not treated. CCyR means the test did not find any cells with the Ph+ chromosome (the mutated gene found in Ph+ CML).
Of the people taking Bosulif, 47.2% had an MMR and 77.2% had a CCyR at 12 months. (This means that no cancerous cells were found in their blood, and they had no symptoms of cancer.) Of the people taking Gleevec, 36.9% had an MMR and 66.4% had a CCyR at 12 months.
The full results of this clinical study will be available once the people within the study have been followed for up to 5 years.
Effectiveness for previously treated Ph+ CML
Bosulif has also been found to be effective for treating Ph+ CML that’s resistant to treatment. (This means you no longer benefit from other treatments or your disease fails to respond to a certain therapy.) This resistance can occur at any time during treatment, even if you’ve been taking your medication for years. People who can’t tolerate their current treatment because of side effects can also take Bosulif for Ph+ CML.
In one clinical study, adults with Ph+ CML that was resistant or intolerant to other drugs, including imatinib (Gleevec), dasatinib (Sprycel), and nilotinib (Tasigna), were given Bosulif. Each drug’s effectiveness was measured with a bone marrow test and reported as a major cytogenetic response (MCyR). MCyR means that
By the end of 24 weeks of treatment:
- 40.1% of people who previously took imatinib had an MCyR to Bosulif.
- 25.9% of people who previously took either nilotinib or imatinib and dasatinib had an MCyR to Bosulif.
Off-label use for Bosulif
In addition to Ph+ CML (above), Bosulif may be used off-label. Off-label drug use is when a drug that’s approved for one use is used for a different one that’s not approved.
According to the National Comprehensive Cancer Network (NCCN) guidelines, Bosulif can be used off-label to treat acute lymphoblastic leukemia (ALL). Bosulif contains the drug bosutinib, which belongs to a class of drugs called tyrosine kinase inhibitors (TKIs). This class of drugs specifically targets cancer cells that have the Philadelphia chromosome. Bosulif can only be used in Philadelphia-positive (Ph+) cancers, such as Ph+ ALL.
One study showed that adults with Ph+ CML or ALL that was previously treated responded to treatment with Bosulif. However, the number of people with Ph+ ALL in the study was limited.
There are no known interactions between Bosulif and alcohol.
However, your liver metabolizes (breaks down) both Bosulif and alcohol. Therefore, drinking too much alcohol while you’re taking Bosulif may prevent your liver from breaking down the drug. This could raise the levels of Bosulif in your body and increase your risk for serious side effects, including liver damage.
Both Bosulif and alcohol can cause side effects, such as:
- nausea
- diarrhea
- headache
- fatigue (lack of energy)
Drinking alcohol during your Bosulif treatment could raise your risk for these side effects. If you drink alcohol, talk to your doctor about how much is safe for you to drink while taking Bosulif.
Bosulif can interact with several other medications. It can also interact with certain supplements and foods.
Different interactions can cause different effects. For instance, some interactions can interfere with how well a drug works. Other interactions can increase side effects or make them more severe.
Bosulif and other medications
Below is a list of medications that can interact with Bosulif. This list does not contain all drugs that may interact with Bosulif.
Before taking Bosulif, talk with your doctor and pharmacist. Tell them about all prescription, over-the-counter, and other drugs you take. Also tell them about any vitamins, herbs, and supplements you use. Sharing this information can help you avoid potential interactions.
If you have questions about drug interactions that may affect you, ask your doctor or pharmacist.
Bosulif and drugs that affect the CYP3A4 enzyme
People taking Bosulif should avoid taking it with drugs that can affect an enzyme (a type of protein) called CYP3A4. (This enzyme is important for breaking down drugs in your body.)
Taking these drugs with Bosulif can either increase or decrease the levels of Bosulif or the other drug in your system. This can raise your risk for side effects.
Some examples of these drugs include:
- drugs used to treat fungal infections, such as ketoconazole and fluconazole (which may increase Bosulif levels in your body)
- drugs used to treat bacterial infections, such as rifampin and clarithromycin (levels of which may increase if taken with Bosulif)
Many drugs can affect the CYP3A4 enzyme. Talk with your doctor or pharmacist about all medications you take to help lower your risk of drug interactions.
Bosulif and proton pump inhibitors
People taking Bosulif should avoid taking it with proton pump inhibitors (PPIs). These are drugs used for heartburn, indigestion (upset stomach), and gastroesophageal reflux disease (GERD). Taking Bosulif with these drugs can lower Bosulif levels in your body, making it less effective.
Examples of these drugs include:
- lansoprazole (Prevacid)
- pantoprazole (Protonix)
- omeprazole (Prilosec)
- rabeprazole (Aciphex)
- esomeprazole (Nexium)
- dexlansoprazole (Dexilant)
If you take a PPI and want to use Bosulif, talk with your doctor or pharmacist about possible alternatives to the PPI.
Bosulif and herbs and supplements
Bosulif may interact with supplements that contain grapefruit extract. Taking Bosulif with these products may increase the levels of Bosulif in your body, which could lead to more side effects.
Before starting Bosulif, talk with your doctor about all supplements you take, especially any that may contain grapefruit extract.
Bosulif and foods
Bosulif may interact with certain foods, such as grapefruit or grapefruit juice. Taking Bosulif and grapefruit juice together may increase the levels of Bosulif in your body. This could lead to more side effects. Talk with your doctor if you regularly drink grapefruit juice or eat grapefruits.
Other drugs are available that can treat Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML). Some may be a better fit for you than others. If you’re interested in finding an alternative to Bosulif, talk with your doctor. They can tell you about other medications that may work well for you.
Note: Some of the drugs listed here are used off-label to treat these specific conditions.
Alternatives for Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML)
Examples of other drugs that may be used to treat Ph+ CML include:
Talk with your doctor if you’re interested in trying a different drug to treat Ph+ CML.
You may wonder how Bosulif compares to other medications that are prescribed for similar uses. Here we look at how Bosulif and Gleevec are alike and different.
Ingredients
Bosulif contains the drug bosutinib. Gleevec contains the drug imatinib.
Uses
The Food and Drug Administration (FDA) has approved both Bosulif and Gleevec to treat certain types of blood cancers.
Both Bosulif and Gleevec are FDA-approved to treat:
- newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in adults*
- Ph+ CML in adults who’ve tried a previous treatment that either didn’t work or caused negative side effects that required stopping treatment
In addition, Gleevec is FDA-approved to treat Ph+ CML in children. (Bosulif is only approved for use in adults.)
Gleevec is also approved to treat these other types of cancer:
- Ph+ acute lymphocyte leukemia (ALL)
- bone marrow cancers, such as myelodysplastic syndrome and myeloproliferative disease
- hypereosinophilic syndrome or chronic eosinophilic leukemia (a group of blood disorders characterized by high numbers of a blood cell called eosinophils)
- mastocytosis (a condition in which cells called mast cells build up in the skin and internal organs)
- certain types of skin cancer
- Kit-positive gastrointestinal (stomach) cancer
* For this use, Bosulif received
Drug forms and administration
Both Bosulif and Gleevec come as a tablet you take by mouth. Bosulif is taken once a day with food. Gleevec is taken either once or twice a day, depending on your dose.
Side effects and risks
Bosulif and Gleevec have some similar side effects and others that differ. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Bosulif, with Gleevec, or with both drugs (when taken individually).
- Can occur with Bosulif:
- shortness of breath
- low appetite
- Can occur with Gleevec:
- muscle cramps or pain
- sleepiness
- blurred vision or other problems with your eyes
- hair loss
- Can occur with both Bosulif and Gleevec:
- diarrhea
- rash
- coughing
- fever
- flu
Serious side effects
These lists contain examples of serious side effects that can occur with Bosulif, with Gleevec, or with both drugs (when taken individually).
- Can occur with Bosulif:
- blood disorders, including thrombocytopenia (low levels of platelets), anemia (low level of red blood cells), and neutropenia (low levels of white blood cells)
- Can occur with Gleevec:
- bleeding problems
- problems with your eyes, such as swelling, blurred vision, dry eyes, and irritation
- gastrointestinal perforations (holes in your stomach or intestines)
- low thyroid hormone levels
- tumor lysis syndrome (when cancer cells release harmful chemicals into your blood)
- serious skin problems, such as Stevens-Johnson syndrome (including rashes and blistering)
- Can occur with both Bosulif and Gleevec:
- heart problems, including heart failure
- liver damage or liver failure
- gastrointestinal toxicity (severe stomach problems), including severe nausea, diarrhea, or vomiting
- kidney damage or kidney failure
- edema (fluid buildup in your body)
Effectiveness
Bosulif and Gleevec have different FDA-approved uses, but they’re both used to treat:
- newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in adults
- Ph+ CML in adults who’ve tried a previous treatment that either didn’t work or caused negative side effects that required stopping treatment
Effectiveness for newly diagnosed Ph+ CML
For the use of treating newly diagnosed Ph+ CML in adults, Bosulif received
The ongoing clinical trial compares Bosulif and imatinib (Gleevec) in people who were diagnosed with Ph+ CML and haven’t received treatment for their cancer before. The trial is set to continue for up to 5 years before there are final results, but some results were reported after the first year.
Bosulif’s and Gleevec’s effectiveness is measured with bone marrow tests. These tests take bone marrow samples and count the number of cells that remain in the body after treatment. In this clinical trial, responses were reported as major molecular response (MMR) and complete cytogenetic response (CCyR). MMR tests bone marrow at the genetic level. This is more specific than CCyR, which tests it at cellular level.
MMR means the level of cells with the BCR-ABL gene (the mutation that causes chromosomes to be Ph+) was at least 1,000 times less than the levels of a person with CML who was not treated. CCyR means the test did not find any cells with the Ph+ chromosome (the mutated gene found in Ph+ CML).
Of the people taking Bosulif, 47.2% had an MMR and 77.2% had a CCyR at 12 months. (This means that no cancerous cells were found in their blood, and they had no symptoms of cancer.) Of the people taking Gleevec, 36.9% had an MMR and 66.4% had a CCyR at 12 months.
The full results of this clinical study will be available once the people within the study have been followed for up to 5 years.
Effectiveness for previously treated Ph+ CML
Bosulif and Gleevec have not been directly compared in adults with Ph+ CML who’ve tried previous treatment. However, studies have found both Bosulif and Gleevec to be effective for treating Ph+ CML in this group.
Costs
Bosulif and Gleevec are both brand-name drugs. There is currently no generic form of Bosulif, but a generic version of Gleevec is available under the name imatinib mesylate. Brand-name medications usually cost more than generics.
Bosulif is significantly more expensive than Gleevec and its generic version, imatinib mesylate. The actual price you’ll pay for any of these drugs depends on your insurance plan, your location, and the pharmacy you use.
Bosulif and Sprycel are prescribed for similar uses. Here’s a look at how these drugs are alike and different.
Ingredients
Bosulif contains the drug bosutinib. Sprycel contains the drug dasatinib.
Uses
The Food and Drug Administration (FDA) has approved both Bosulif and Sprycel to treat certain types of blood cancers.
Both Bosulif and Sprycel are FDA-approved to treat:
- newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in adults*
- Ph+ CML in adults who’ve tried a previous treatment that either didn’t work or caused negative side effects that required stopping treatment
In addition, Sprycel is FDA-approved to treat newly diagnosed Ph+ CML in children. (Bosulif is only approved for use in adults.)
* For this use, Bosulif received
Drug forms and administration
Both Bosulif and Sprycel come as a tablet you take by mouth. Bosulif is taken once a day with food. Sprycel is taken once a day, either in the morning or the evening. Sprycel can be taken with or without food.
Side effects and risks
Bosulif and Sprycel have some similar side effects and others that vary. Below are examples of these side effects.
More common side effects
These lists contain examples of more common side effects that can occur with Bosulif, with Sprycel, or with both drugs (when taken individually).
- Can occur with Bosulif:
- fever
- flu
- coughing
- low appetite
- Can occur with Sprycel:
- weakened immune system
- bleeding
- muscle pain
- bone pain
- Can occur with both Bosulif and Sprycel:
- edema (fluid buildup in your body)
- nausea or vomiting
- rash
- headache
- diarrhea
- shortness of breath
- fatigue (lack of energy)
Serious side effects
These lists contain examples of serious side effects that can occur with Bosulif, with Sprycel, or with both drugs (when taken individually).
- Can occur with Bosulif:
- gastrointestinal toxicity (severe stomach problems), including severe nausea, diarrhea, and vomiting
- heart failure
- Can occur with Sprycel:
- high blood pressure in the lungs long QT interval (abnormal electrical activity in the heart that can lead to abnormal heart rate or rhythm)
- ischemic heart attack (lack of oxygen to heart muscles)
- tumor lysis syndrome (when cancer cells release harmful chemicals into your blood)
- bleeding problems
- severe skin reactions
- Can occur with both Bosulif and Sprycel:
- liver damage or liver failure
- blood disorders, including thrombocytopenia (low levels of platelets), anemia (low level of red blood cells), and neutropenia (low levels of white blood cells)
- kidney damage or kidney failure
- edema (fluid buildup in your body)
Effectiveness
Bosulif and Sprycel have different FDA-approved uses, but they’re both used to treat:
- newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML) in adults
- Ph+ CML in adults who’ve tried a previous treatment that either didn’t work or caused negative side effects that required stopping treatment
These drugs haven’t been directly compared in clinical studies, but studies have found both Bosulif and Sprycel to be effective for treating Ph+ CML.
Costs
Bosulif and Sprycel are both brand-name drugs. There are currently no generic forms of either drug. Brand-name medications usually cost more than generics.
Bosulif and Sprycel prices will vary depending on your prescribed dose. The actual cost will also depend on your insurance plan, your location, and the pharmacy you use.
You should take Bosulif according to your doctor’s or healthcare provider’s instructions. Bosulif is a tablet that is taken once a day by mouth with food.
When to take
Bosulif should be taken once a day with food. It can be taken at any time of day, but you should take it around the same time each day.
To help make sure you don’t miss a dose, try setting a reminder on your phone. A medication timer may be useful, too.
Taking Bosulif with food
Bosulif should be taken once a day by mouth with food.
Can Bosulif be crushed, split, or chewed?
No, Bosulif should never be crushed, split, or chewed. It should always be taken as a whole tablet.
Bosulif contains the drug bosutinib, which belongs to a class of drugs called tyrosine kinase inhibitors (TKIs). This class of drugs is used to treat specific types of cancers, such as Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML).
In Ph+ CML, the cells that make up your white blood cells contain abnormal DNA (genetic material) that’s called the Philadelphia chromosome. When cells with abnormal DNA replicate (make more cells), they make abnormal cells, which are sometimes cancerous. The buildup of abnormal cells can cause problems with how your body functions.
In Ph+ CML, the Philadelphia chromosome causes your body to make too many white blood cells. These white blood cells are immature and abnormal, so they can’t function as they should in your body. These white blood cells also take up room inside your body. This doesn’t allow your body to make healthy, normal blood cells that do function properly.
Bosulif works by attaching to and blocking a protein called tyrosine kinase. This protein usually sends signals to your white blood cells and tells them to multiply and grow. When the protein is blocked and can’t signal to your blood cells, the abnormal (cancerous) blood cells die. This allows your body to make healthy, normal blood cells that work properly.
How long does it take to work?
Bosulif can take different amounts of time to work in different people. Some people see an improvement in their cancer as soon as 3 months after starting Bosulif.
Your doctor will order lab tests after you’ve taken Bosulif. These tests will help show if Bosulif is working for you. In clinical studies, people taking Bosulif had a decrease in the number of cancer cells at 24 weeks, 48 weeks, and 12 months.
You should not take Bosulif if you are pregnant. Bosulif has not been studied in pregnant women. However, in animal studies, Bosulif use during pregnancy caused fetal harm.
If you’re pregnant, your doctor may have you wait until you’ve given birth to start taking Bosulif. They may also recommend a different drug that you can take while pregnant.
It’s unsafe to take Bosulif during pregnancy. If you’re sexually active and you or your partner can become pregnant, talk with your doctor about your birth control needs while using Bosulif. You should continue using birth control for at least 2 weeks after you stop taking Bosulif.
It’s not safe to breastfeed while taking Bosulif. There haven’t been any human studies in women taking Bosulif while breastfeeding. However, animal studies showed that it can pass into breast milk. If you take Bosulif and plan to breastfeed, you should wait at least 2 weeks after your last dose of Bosulif to begin breastfeeding your child.
Here are answers to some frequently asked questions about Bosulif.
Why can’t I get Bosulif at my local drugstore?
Bosulif is only available at specialty pharmacies. These are pharmacies that are authorized to carry specialty medications. (Specialty medications are drugs that are complex, have high prices, are difficult to take, or have special dosage or storage requirements.)
Pharmacists at specialty pharmacies are trained to be experts in certain areas of medicine. These pharmacists can help you figure out your insurance coverage for certain treatments. They can also help monitor you for side effects while you’re using certain medications.
Will I need any tests before I can start taking Bosulif?
Your doctor may order some tests before you start Bosulif, depending on whether you’re taking Bosulif for newly diagnosed Philadelphia chromosome-positive (Ph+) chronic myeloid leukemia (CML), or whether you’re being switched from another therapy because it didn’t work for you.
Examples of blood tests your doctor may order include:
- Complete blood count. This test checks the level of each type of blood cell in your body. Your doctor might order this test before you start taking Bosulif, and then every few months once you start taking Bosulif. This test helps your doctor make sure that all of your blood cell levels are in a safe range.
- Liver function tests. These tests check your liver enzymes (a type of protein) before and during your treatment. The tests help your doctor make sure that your liver stays healthy during your treatment with Bosulif.
- Kidney function tests. These tests check your kidney function and help your doctor make sure that your kidneys stay healthy during your Bosulif treatment.
Your doctor may want you to have other tests done as well. These may be done before or during your Bosulif treatment.
Is Bosulif a type of chemotherapy?
Bosulif is not a form of chemotherapy (traditional drugs used to treat cancer). It works differently than chemotherapy in your body.
Chemotherapy affects cells in your body that are rapidly growing (making more cells). Chemotherapy affects cancer cells, but it can also affect some of your normal, healthy cells.
Bosulif is a targeted therapy. It only attacks a specific type of cancer cell. It doesn’t affect all the rapidly growing cells in your body.
Because chemotherapy can affect all of the rapidly growing cells in your body, it can cause more side effects than targeted therapies do.
Will Bosulif cure my CML?
There is currently no cure for chronic myeloid leukemia (CML). However, in many cases, a targeted therapy (such as Bosulif) can
CML has three phases: chronic phase, accelerated phase, and blast phase. With each of these phases, there’s a certain number of cancer cells in your body.
Most people are diagnosed with CML in the chronic phase, which means they have
The National Comprehensive Cancer Network (NCCN) has the following recommendations for treatment goals for CML, based on the level of cancer in your body. If the treatment is working:
- After 3 to 6 months of treatment, you should have less than 10% cancer cells in your blood.
- At 12 months after starting treatment, you should have less than 1% cancer cells in your blood.
- After 12 months of treatment, should have less than 0.1% cancer cells in your blood.
Taking Bosulif gives me diarrhea. How can I treat it?
Your doctor may recommend some ways to help treat diarrhea caused by Bosulif. Examples of things you can try at home include:
- Taking loperamide (Imodium). This over-the-counter medication may help relieve your diarrhea. However, check with your doctor before taking it.
- Staying hydrated. Drinking plenty of water or fluids with electrolytes (such as Pedialyte) can help you stay hydrated if you’re having diarrhea.
- Changing your diet. Avoiding caffeine, alcohol, or dairy may help relieve diarrhea.
Call your doctor right away if you experience seven or more loose stools per day, pain, or blood in your stool while taking Bosulif.
Before taking Lupron Depot, talk with your doctor about your health history. Lupron Depot may not be right for you if you have certain medical conditions or other factors affecting your health. These include:
- Allergies to Bosulif. You should not take Bosulif if you have a history of allergies to this drug. Some people have had anaphylactic reactions (severe allergic reactions) when taking Bosulif.
- Heart disease. If you have heart disease, talk with your doctor about whether Bosulif is safe for you. Although it’s not common, some people who take Bosulif can develop heart failure. Your doctor will likely monitor your heart function while you take Bosulif.
- Liver disease. If you have liver disease, talk with your doctor about whether Bosulif is safe for you. It’s not common, but some people who take Bosulif can develop liver damage. Your doctor will likely monitor your liver function while you take Bosulif to make sure your liver enzymes (a type of protein) are at safe levels.
- Kidney disease. If you have kidney disease, talk with your doctor about whether Bosulif is safe for you. It’s not common, but some people who take Bosulif can develop mild to severe kidney damage. There have also been reports of kidney failure while taking Bosulif. Your doctor will likely monitor your kidney function while you take Bosulif to make sure your kidneys are working properly.
- Pregnancy. Bosulif is not safe to use during pregnancy. For more information, see the “Bosulif and pregnancy” section above.
- Breastfeeding. It’s not safe to take Bosulif while breastfeeding. For more information, see the “Bosulif and breastfeeding” section above.
Note: For more information about the potential negative effects of Bosulif, see the “Bosulif side effects” section above.
Do not take more Bosulif than your doctor recommends.
What to do in case of overdose
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or go to the nearest emergency room right away.
When you get Bosulif from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee the medication will be effective during this time. The
Storage
How long a medication remains good can depend on many factors, including how and where you store the medication.
Bosulif tablets should be stored at room temperature between 68°F and 77°F (20°C and 25°C) in a tightly sealed container away from light. Avoid storing this medication in areas where it could get damp or wet, such as bathrooms.
Disposal
If you no longer need to take Bosulif and have leftover medication, it’s important to dispose of it safely. This helps prevent others, including children and pets, from taking the drug by accident. It also helps keep the drug from harming the environment.
You should not touch or handle crushed or broken tablets.
The
The following information is provided for clinicians and other healthcare professionals.
Indications
Bosulif (bosutinib) is FDA-approved to treat the following conditions in adults:
- newly diagnosed chronic phase Ph+ chronic myelogenous leukemia (CML). This indication is approved under an accelerated approval for an ongoing study based on molecular and cytogenic response rates at 12 months.
- chronic, accelerated, or blast phase Ph+ CML with resistance or intolerance to alternate therapy
Mechanism of action
Bosulif is a tyrosine kinase inhibitor (TKI). It works by inhibiting various forms of BCR-ABL kinase, an enzyme that promotes CML. In lab rat cells, Bosulif was shown to inhibit 16 of 18 forms of BCR-ABL kinase that were resistant to imatinib.
Pharmacokinetics and metabolism
Bosulif exhibits peak concentration at 6 hours following a single oral dose, with absolute bioavailability at 34%. When given with a high-fat meal, Bosulif maximum concentration (Cmax) and area under the curve (AUC) increased 1.8-fold and 1.7-fold, respectively.
Bosulif is 94% to 96% protein-bound, independent of concentration. Following a single oral dose of Bosulif, the mean half-life was 22.5 hours. Bosulif is metabolized by CYP3A4 and mostly eliminated through feces.
Contraindications
Bosulif is contraindicated in patients who have a history of hypersensitivity to Bosulif.
Storage
Bosulif tablets should be stored at room temperature between 68°F and 77°F (20°C and 25°C), with some flexibility for transportation between 59°F and 86°F (15°C and 30°C).
Procedures for proper disposal of anticancer drugs should be considered. Bosulif should not be touched or handled if crushed or broken.
Disclaimer: Medical News Today has made every effort to make certain that all information is factually correct, comprehensive, and up to date. However, this article should not be used as a substitute for the knowledge and expertise of a licensed healthcare professional. You should always consult your doctor or other healthcare professional before taking any medication. The drug information contained herein is subject to change and is not intended to cover all possible uses, directions, precautions, warnings, drug interactions, allergic reactions, or adverse effects. The absence of warnings or other information for a given drug does not indicate that the drug or drug combination is safe, effective, or appropriate for all patients or all specific uses.